Thanks @Isaiah_40_31 , so hard to know what’s right or wrong until you’ve done with this condition has been my experience - for better or worse but normally worse unfortunately! I’ve been I quite a bit of pain around the incision this afternoon/evening (it’s gone a tiny bit lumpy) so perhaps I overdid it today with the massage. Will try less of the direct contact tomorrow and see if it’s any better. Good thing I’ve got all that stomach acid though for the other possible issues. Haha
Unless it’s maybe a swollen & infected/ stone in your salivary gland & the massage is releasing that a bit? Not sure exactly where you’re massaging if there’s the parotid gland in that area?
@BraveKat - We’ve had a few members who ended up being allergic to the internal dissolving sutures that are sometimes used for closing the incision. One member had a stitch surface 2 years after her ES surgery. I’m wondering if you had internal dissolving sutures if they could be part of the problem, i.e. they haven’t dissolved like they should & are causing the irritation you feel in your incision & surrounding area.
Please let me know how you get on and if you feel like it was too much. I was thinking the direct zigzag/circular motions over the incision was a bit much but when I woke the next morning it actually felt like blocked up. I am also on some antibiotics (a different ED visit for now swelling in the opposite arm - luckily not a blood clot). They seem to be helping my neck which is where I imagine the infection is. But will save that for conversation for the ENT.
Did your doctor talk to you about slowing of drainage from the area post surgery as a result of removing lymph nodes at all? I didn’t have any removed but I feel like some might be trapped between the incision and my jaw bone. That’s where the lumps/pain started the night of the self massage. That’s also where the pain post surgery was. Everyone says there scar is numb. But mine has been painful since day one.
It’s hard to say but it might be the base of the parotid gland (pain definitely spreads to the whole area when the pain in acute). But also I think it’s the submandibular gland. From where it appears to be positioned in diagrams of the head, I think my incision may be right on the base of it and the stitches/new tissue might be constricting it. That’s the generally feeling. There has been pain and lumpiness there since the surgery. It’s definitely reduced slowly over the last 7 months but this is now my 4 course of antibiotics in that time. One infection took 1 month to clear and that’s when I got the red bumpy rash on the skin.
Not sure how the infection taste in the mouth relates to it but maybe the swelling from poor drainage is pressing tissue together inside my face and it’s rubbing and trapping bacteria and then dripping down. I’m noticing it less after 5 days of the antibiotic course but I think structurally something isn’t sitting right.
Fingers crossed I can get to the ent soon to get an examination done.
Yes could be that too. Thank you!
Either way, I just feel that the incision was made too close to the underside of the jaw. The pressure between the top of the incision and the jaw post surgery didn’t seem right and it’s generally lumpy in and around the incision now - not the incision/scar itself but just under that, maybe the lymph system. My doctor did say swelling could tether things post surgery but if the glands aren’t free to move, I would imagine the healing process could be that much slower.
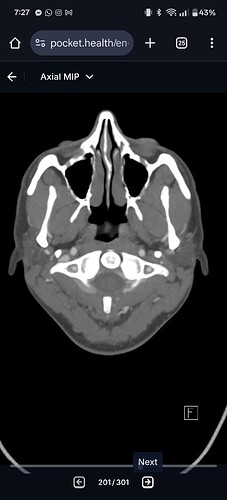
@maryscooter are you able to post some axial views of the CT? Even though you’ve already had styloidectomies and c1 shaves, I’m particularly interested in seeing your c1 in axial view, and your hyoid bone in axial view. I’ve uploaded two images from my CT to help you locate the two areas. I’m particularly interested in your hyoid as it’s looking like it could be deep in the front view you’ve shown us. And I want to see if it’s digging into anything important! The glossopharyngeal nerve runs along the carotid sinus area of the internal carotid and my hyoid is rubbing against it and causing the left side face numbness and burning (like a perfect line dividing my face and throat in half like you said). Just go down the axial view until you see your horseshoe shaped hyoid bone and see where the tips of the hyoid are resting!
Actually @maryscooter if youre able to screen record you scrolling through the axial view from skull base all the way to the top of the chest that would be best! I’m becoming quite good at reading the axial view of cervical CTs!
The drawback to the 3D models is that it can be easy for some structures to hide behind others making it difficult to see everything.
@TML - That’s one of my biggest shortfalls on this forum is not being able to read the axial views of cervical CTs how have you learned to read them & understand what you’re seeing?
@Isaiah_40_31 takes some practice but once you get the hang of it it’s like riding a bike!
When my symptoms started in September and I wasn’t getting answers from doctors I finally got my hands on my CT imaging in January or February. I originally thought I had something wrong with my atlantoaxial joint because I had cracked my neck while sleeping with my head turned back in September. To look for malrotation of C1 and C2, radiologists often use the axial view for measurements, so that’s how I first got familiar with axial. Then I sent my CT for second opinion because I thought my C1 and C2 did look malrotated but the radiologist assured me that they aren’t (they are all sort of rotated, but rotated with each other, not off each other). So from there I was already familiar with axial view at least in terms of the upper cervical vertebrae. After that disappointment I went back to the axial view at C1 and decided to look for vascular structures because my symptoms are worse with head movements (and vertebrae were ruled out based on second opinion so I figured a vein/artery or maybe nerves were getting compressed with movement). It was then that I discovered my IJVs crammed between the styloids and C1. I then learned to follow each vascular structure from C1 all the way down to the collarbones. Once you follow each structure the full length in axial view, most CTs look similar. If you can locate the structure at the skull base it’s pretty hard to lose it when traveling down (unless they lose contrast, but even then you can still faintly locate them). I find that axial view is best because you can fully assess the full length of a vascular structure, rather than it just popping in and out of frame in say the coronal view!
Thx for your explanation, @TML. I know that doctors prefer looking at the CT slices for the reason you mentioned,
and I’ll add - also a bony structure. I think that looking at both the axial/transverse views, & 3D sagittal/coronal views may help give a more complete picture of “the story”.