Hi@NRuflove so so so much appreciate you typing this out like this, gosh its a big bill for one test! but I know how important it is… I have very similar symptoms to you and am to living in a chair/ sleeping in to manage symptoms… I also have bad vision & cognition so typing & following chats so difficult… just been trying to catch up with your progress… I just thought of saying that I think the US specialists mention that anaesthesia can change results on pressure measurements but I may have gotten that confused with the LP test im sorry I can’t remember… maybe someone else will know more… well done for getting as far as you have and being so strong with your other half too to stand your ground and ask all those questions during the follow up… xx
Hi @LivvySheep
Thanks for your message. Since my last update, I’ve had the further cross-sectional imaging that the INR requested following my catheter venogram, by way of dynamic CT venogram with contrast. The report from this concluded that this imaging was congruent with the recent catheter venogram and there was no significant evolution since my previous CTV in 2018. Furthermore, there was no clear evidence to support functional venous obstructions.
My follow-up consultation with Mr Hughes was very brief. He informed me that my imaging does not support a diagnosis of ES. We again discussed my abnormal venous system and the high pressures shown in the catheter venogram and I reminded him of how severely incapacitated I now am with my symptoms. He acknowledged my quality of life was poor and agreed to refer me to Mr Toma (neurovascular consultant) at CCL to discuss whether my abnormal venous system could be to blame. That appointment is scheduled for mid-August. Seeing as the INR @ CCL reported the scans as normal, I don’t for one second think Mr Toma is going to offer any assistance at all but will happily take £300 for a 15 minute consultation just to tell me he can’t help me!
In the meantime, when I was seeing Mr Vajramani (a private neurosurgeon who deals with pain relief) last year, who thought I had occipital neuralgia so was treating me with nerve blocks in my head/neck (unsuccessfully!), he referred me to his clinic in the NHS and, finally, that appointment was a few days ago. Bearing in mind Mr Hughes (ENT at CCL) had by now said I do not have ES, I went along to my appointment with Mr Vajramani who was shocked to see me because he was the consultant who, whilst injecting nerve blocks in my head/neck, had originally palpated the large bony lump in my neck and subsequently referred me for a CT scan that confirmed I had bilateral elongated and thickened styloids, reported as being in keeping with ES. Mr Vajramani then transferred my care over to Mr Patel (a private ENT consultant), who was useless, hence latterly, my-self referral to Mr Hughes at CCL.
I updated Mr Vajramani with the news that Mr Hughes felt my imaging did not support a diagnosis of ES (even though my original CT from Dec 2022 quite clearly says my elongated and thickened styloids are in keeping with a diagnosis of ES!). Satisfied that Mr Hughes had confirmed ES wasn’t the cause for my neck/head pain, he was happy to start with a nerve block injection around the site of the left styloid. He asked me to lie down on my R side and felt my neck. He immediately palpated the bony lump on the L side of my neck and said he couldn’t understand how Mr Hughes was unable to palpate the lump himself as it was so prominent. I offered him the disk with my recent imaging from CCL and he said he would review this himself later on. He proceeded to inject the nerve block over the site (which hasn’t helped at all) and agreed to see me again in 6-8 weeks. By that time, I would also have seen the private neurovascular consultant at CCL to discuss my abnormal venous anatomy and he would hopefully have viewed my recent imaging.
My problem now is that I know there is something not right in my neck. I can feel it rubbing inside (and have done for many years) but I cannot get anyone, other than Mr Vajramani, to take me seriously. I hope he views my imaging before our next appointment and is able to view the exact area where the bony lump is, and either rule it in or out as an issue.
Anyway, to try and move things forward quickly, I have a telehealth appointment with Dr Patsalides in the US in late September who will review my imaging and give me his opinion. I chose him primarily because I want to know if my abnormal venous system is the cause of my headaches/neck pain. If he feels not, then I will be back to the drawing board and may try seeing Mr Axon privately.
Best wishes.
Nicky
Costs mentioned in this message are:
Dynamic CT head/neck with contrast @ CCL = £997
X2 follow ups with Mr Hughes (ENT) @ CCL - £260 each so £520
Follow up with Mr Toma (neurovascular consultant) due in mid-August @ CCL = £300
Telehealth appointment with Dr Patsalides in the US - £200
So sorry that you’re having so much difficulty getting someone to treat you, it’s crazy, even with paying privately! I hope that you get somewhere with your upcoming appts. I think he was going to to more studying, so not sure if he’s doing any consulting now, but some members have sent scans to Kjetil Larsen Home - MSK Neurology I don’t know if that might be helpful ![]()
Sending you a hug ![]()
Gosh bless you you’ve been round the houses and back again and had to pay for the trouble and all whilst being so poorly, im so sorry NRuflove. Thank you for taking the time and effort to share your experiences with the forum. It does seem very strange how Mr.H doesn’t think its ES? I hope you get some more validation through the NS you are seeing and also some more answers about your high pressures from a specialist in VES in the US, it would be a start just know what we are dealing with I know… Have you ever been tested for IIH or eye problems considering you can’t lie flat? Surely Mr.Axon would be interested to help you simply on the basis of classic ES? I really hope you get some answers soon considering all the money you have had to spend so far. Just to say that I admire your strength and spirit.
I am due to see Prof.Matharu at Queens (neuro) in a few weeks and also to speak to rob Pattinson pt in Bristol for a follow up for nTOS. He said to me he has seen patients have improvement with headaches when treating the TOS. My arms go completely numb just absolutely dead no feeling in them when I sleep which could poss be released to TOS. Not that I sleep much with these headaches. Its interesting to say that your NS thought you had occipital neuralgia yet the nerve blocks done work - that would suggest it isn’t that?
Best wishes to you too.
Hello, am so sorry to read about your severe health problems & failure of medics to help you. sadly not an uncommon situation in UK. dont give up.
I have copied your pressures below, so I can add some observations. I think you need an urgent referral by GP to Queen’s Square and maybe go to see Mr Watkins privately (only £150 for consult). your pressures are high and he may be able to offer help/diagnostics and Queens Sq private ward is MUCH cheaper £ than Cleveland.
So Mr Watkins at Queens Sq has told me “normal pressure” is between 0 and 20, a lot of your left side pressures are above 20, which is abnormal. the report you shared has very few results on the right side of your brain and report says that access could not be gained to most of right side. if they can’t access the right side then how can they truly know what gradient differences in fact exist inside your brain. they use gradient differences because our brain pressures vary and so finding a gradient difference is a material finding they use. but they can’t do that for you if no access to right side possible. I had a problem in accessing my right side before all my surgeries too. Qs say IHH threshold is 30, but I know my highest pressure of 20 in my right sigmoid sinus is anything but normal and causes me a world of pressure and pain (my pressures post surgeries are between 14 and 20 if helps). But had to pay to prove this 20 pressure was an issue and show gradient difference before they agreed to help. its rubblish. I view imaging etc reports with suspicion now and look for what is not there as much as what is reported on. I ask for missing information, it annoys them but they do it.
they only stent for a gradient difference of 5 or more (not gradient of 1 like I have). we cannot see your gradients without right side measurements being obtained but left side pressures are too high as over 20. you will have to be firm with them but its the only way you can get some help to improve things. I really sympathise with your situation. I could not see you posted any imaging about possible styloid compression of JV area but good to share it if able for member input. I had doctor screenshot image of JV compression or you can ask for copy of images and look at them yourself/post them here for member input. None of us are medics but we have all seen a lot of imaging showing compression of JVs between c1/styloid as VES patients.
hope that is some help. Take care. D
I suspect the pressures done in UK are in centimeter of water (cm H2O) instead of millimeter of mercury (mm HG) as the ones done in US & Canada. The reason I came to this conclusion is all the studies I read in UK by Higgins are in this unit format ( An example screenshot is shown below). 1 mm HG in (0 Degree C) is equivalent to ~ 1.36 cm H20 ( in 4 Degree C). This is because a column of water is 13.6 times higher than column of mercury which exerts the same pressure (mercury has higher density) so 13.6 cm H20 pressure reading is equivalent to 1 cm HG pressure but since US & Canada use mm HG instead of cm HG, we need to divide 13.6 by 10 since 1 cm = 10 mm, so you need to divide 1.36 to the UK measurements to get an equivalent to mm HG. So I assume her highest pressure reading (24 with assumed unit of cm H2O) will be equivalent to 17.6 mm HG (24/1.36). This should be confirmed by @NRuflove with her interventional radiologists but I believe it is the standard in UK.
Here is the example from Higgins study below

Hi D
Thank you for your message. I hope you’re feeling as well as you can in the circumstances.
Mr Hughes is adamant that the INR (Dr Peter Cowley) did not think my pressures were high or require any further investigation. It was only when I expressed to him how awful my life currently is that he agreed to refer me to Mr Toma (neurovascular consultant) at CCL and I’m due to see him in a few weeks.
With CCL being so expensive (and their admin being very poor), I searched for an alternative consultant and found Mr Laurence Watkins @ QS. About a month ago, I made contact with Mr Laurence Watkin’s secretary, Ashleigh @ QS. She asked me to send her my most recent correspondence with Mr Hughes as well as imaging files and reports. These were submitted to her without delay. Several weeks’ passed and I didn’t hear back so I sent her a polite reminder expressing that I’d like a private appointment. Ashleigh replied to say she would speak to Mr Watkins. That was a few weeks ago and I’ve still heard nothing. I’m presuming he isn’t go to see me but wish he would tell me that.
I also have an appointment in late September with Dr Patsalides for a second opinion. Even if I don’t have ES or VES, that’s fine, but perhaps he can give some guidance as to how I can move forward with the pressure issues I seem to have and my left sided neck pain.
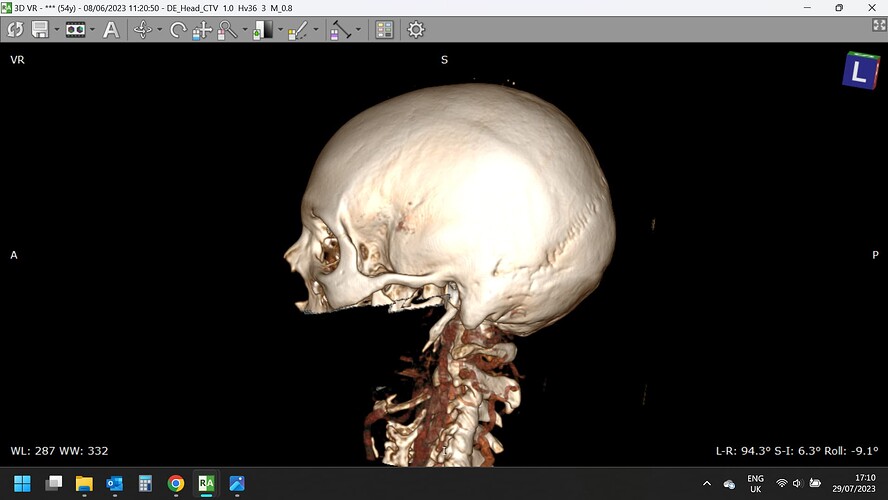
I’ve attached a few images. I’m not sure if the quality is sufficient for anyone to see but you can certainly see my styloids ![]() .
.
Once again, thank you to everyone for the help and advice. I won’t give up - I can’t because I would like my life back.
Nicky
Hi KoolDude
At the time of undergoing the catheter venogram procedure, I knew absolutely nothing about it, hence why I was listening so carefully which is how I heard Dr Cowley talk about millimetres of mercury so have presumed that is the unit used for my measurements. I did request clarification but it has not been forthcoming but bearing in mind what you’ve said, I will make another request.
Nicky
Hi Nicky
I suggest you just ask Ashleigh for next available appointment and just book it.
Peter Cowley is based at QS and did my first Venogram end 2021. Like you he could not access most of right side of my brain then.
Will see if can add anything when on desktop next. D
Hi again, notice your comment about “want your life back”. Was there an event/circumstance that was a trigger for your ill health problems? I ask as if so that may be relevant to diagnosing your problems. D
Hi D
No, no event. Things were bad as far back as 2010 and gradually pain and frequency of headaches increased. One night in early 2018, I went to bed and, wham - overnight my health fell off a cliff with disabling head and neck pain and I’ve been fighting for an answer ever since. I’ve had all the usual responses - it’s migraine, chronic fatigue, fibromyalgia, and depression is one of their favourite diagnoses ![]() but I know something isn’t right in my neck and head so will fight on.
but I know something isn’t right in my neck and head so will fight on.
@NRuflove - One thing few doctors seem to take into consideration is that even when there is a “normal range” for something, there are always a few outliers - those people who’s normal range is lower or higher than what the docs consider normal. I’m really sorry for the way you’ve been dismissed regarding your possible vascular compression especially since your right side couldn’t be accessed. To me that would indicate complete or almost complete blockage or at least a solid reason to investigate further to see why it was inaccessible!
Your styloids are immensely long & the left side is very thick. I don’t know how any doctor who knows anything about ES could dismiss that diagnosis in your case. With thick styloids often comes vascular compression.
I like @PatientD 's advice - “I suggest you just ask Ashleigh for next available appointment and just book it.”
Those styloids look nasty & I can’t understand why no-one is taking this seriously…my heart goes out to you with the fight you’re having, sending you hugs & praying for you ![]()
![]()
Hi
Following @KoolDude’s thought that my cerebral catheter venogram and manometry pressure readings may well be in cmH20 and not mm Hg, I checked with CCL and they confirmed they are mm Hg.
I had a private appointment yesterday with Mr Axon in Cambridge. He looked briefly at my imaging, examined me, asked me lots of questions and then said I do not have Eagle Syndrome. Despite having throat pain/discomfort and a large bony protruding lump behind/below my left ear, he said that the main symptom for ES is the styloid popping through or being palpable in the back of the mouth internally, making it very painful to eat combined with sharp pain into the ear and jaw.
I asked him what the bony lump protruding from behind/below my left ear was and he said it was the C1 transverse process and it was normal for it to protrude as far as mine although not his area of expertise. Aside from my throat discomfort and swallowing issues, this is where a lot of my pain emanates from which in turn results in a dreadful headache and a feeling of pressure. I then asked what was causing my throat issues but he didn’t have an answer. I mentioned that my CT report stated the length and thickness of my styloids were in keeping with a diagnosis of ES, but he said a high proportion of people would have elongated styloids if they were scanned and mine were just over 30mm which is not long and they were not particularly thickened. He flicked up and down a few times through my recent CT head/neck venogram on the axial view and said the report was that there was “no clear imaging evidence to support functional venous obstruction”
He was more interested in my pulsatile tinnitus and we ran through lots of questions about it. He thought my catheter venogram pressure readings were high (the highest being 24mmHg) and said that CSF had to operate at least 3 mm Hg than that, which, he felt, may indicate I have IIH. He seemed surprised that CCL had concluded my pressure readings were okay and that nobody had asked me to visit an optician to have the back of my eyes checked for papilledema and suggested I do so. He also suggested I see a neurologist to discuss my pressure readings (I thought a neurovascular consultant would have been preferable?) but if I did not have papilledema, I probably wouldn’t get a neurologist to take my pain/headaches seriously. However, if I did have papilledema then a neurologist would probably undertake a lumbar puncture and if the pressure did indicate IIH then I would likely be prescribed a few medications - I can’t remember one but the other was Topiramate, which I have been prescribed previously by every neurologist I’ve seen over the years and had absolutely no effect whatsoever – other than my hair fell out.
Whilst he was quick and to the point, he did end the consultation by asking me to keep in touch and let him know what happens next.
I have posted the pictures of my styloids here previously and they don’t look great, however, I’ve now seen the UK’s top ES consultant (according to most people) and he was very quick to tell me I don’t have ES. There isn’t much more I can do in this regard so will have to accept there are no further avenues for me to explore ES in the UK.
I’m due to see Mr Laurence Watkins, neurosurgeon next week to discuss whether my abnormal venous anatomy could be the cause for my high pressures and lots of pain, however, I don’t for one minute think there could be any correlation between my high pressure and throat pain! I may well be wrong but feel I now need a miracle to sort out the mess I am.
I’d like to thank you for the support you have given me and wish you all well on your journeys to better health.
Nicky
I’m so sorry that Mr Axon wasn’t able to help you, along with Mr Hughes, & that you’ve not been able to get any answers for your throat pain…the styloids certainly look thick to me, but obvs we’re not doctors on here! ![]()
I hope that you get some answers from Mr Watkins next week for your headaches at least…Sending you a hug, I feel for you being sent round the houses ![]()
Thanks for Clarifying. If that is the case, you really have venous hypertension based on your DSA readings which are quite high. I wonder if you can see Dr Higgins and show him the result of the DSA. He is good at this sort of thing and wrote many papers on it. He also has the ear of Dr Axon. If he thought that your C1 or Styloid were the culprits, he can easily convince Dr Axon to do the surgery.
I also see that your throat symptoms indicate glossopharyngeal nerve irritation or compression possibly by your Styloids. You also might also have venous compression somewhere ( from the chest to brain sinuses) that needs to be investigated with a great deal of suspicion given your high pressure readings. I would like to see your CTV if you have it on (https://www.dicomlibrary.com/) which is anonymous and easily accessible. I am thinking something was missed here which is common in many venous compressions.
Anyways, I looked at the images you posted, though not clear enough, they do show a sign of collateral drainage ( Cyan Arrows) which indicates that your jugular vein is somewhat impaired and blood gets rerouted to Collateral Veins. I am not a doctor but I also think your Styloids are by no means short. For a comparison, My Styloid was 1.8 CM and it was removed as it was compressing my left Jugular Vein so I am surprised they think it is normal given that yours are ~ 3 CM.
Hi @KoolDude
The CTV contains 4100 slices/files. I’ve zipped it but it won’t upload to dicomlibrary, possibly because of the size. Is there any other app I can use to get it over to you?
Nicky
I had a CTA & MRV which I uploaded to dicomlibrary. The MRV took about 10 hrs to upload because of the number of images. Are you getting an error message from dicomlibrary, or does it just seem like it’s looping which is what I first thought until someone educated me in the number of images it was uploading & anonymizing. My CTA loaded a bit faster, but I don’t know why as it also had a lot of images.
Also, I must say I completely disagree w/ Mr. Axon. ES has many, many more symptoms that define it than the few he’s using as criteria for diagnosing it. Sadly, we’ve found that some of the best ES surgeons filter patients by requiring that certain symptoms be present before they will diagnose ES. I highly recommend that if it’s possible, you get a second opinion from Mr. Hughes in London as we’ve had several members who’ve recently been diagnosed & offered surgery by him. He may have less strict boundaries for ES symptoms recognition. Your styloids are plenty long AND thick enough to be causing ES symptoms, & as @KoolDude noted, vascular compression, or vascular outflow obstruction, as it’s now being called, which your symptoms loudly proclaim.
Hi @NRuflove,
The reason that this fails is usually combination of low upload speed of your internet and the large number of series that you try to upload. I think one way to do this is to export ONLY the series that has the most slices and zip it and then upload it in dicomlibrary. That way you do not have to load all 4100 slices. Generally if you look at the CTV, one series will usually contain few hundred slices (thin slices). That is only the one I need. So you can select that series and export it in dicom format and then zip it and upload. That should take less time to upload and high success rate than trying to upload the whole CTV.
Hi @KoolDude
Hopefully, you’ll be able to see what you want.
https://www.dicomlibrary.com?study=1.3.6.1.4.1.44316.6.102.1.202308131193592.1899224043161747918120
Thank you.
Nicky