Hi @mamaleah30! Sorry for the delay. We moved at the beginning of the month and we are still unpacking things… man now I remember now why I hate moving haha.
I’m sorry to hear that you may also need a stent. Have you had a styloidectomy already? Please let me know how it goes for you.
I saw Dr. Fargen in North Carolina in April and he performed a cerebral angiogram and venogram on me to look at the flow in my left and right jugulars and measure pressure gradients. I was sedated on my back but awake during the procedure, so I could communicate to Dr. Fargen any symptoms during. I could also see my scan on a very large TV next to me and could watch the contrast flow though my venous system as Dr. Fargen inject contrast.
During the procedure he had me orient my head and neck in the neutral, rotated left, rotated right, and chin-tucked positions and measured the pressures at each position. My results showed that I had high pressure gradients in my right and left jugulars when I rotated my head in either direction with the highest gradients occurring in my right jugular, which I have not had a styloidectomy on.
He also performed a provocative test by applying a strong injection of contrast above C1 in each jugular with my head in a neutral position to try to briefly increase the pressure and replicate symptoms. He did this on my right and left jugulars. I felt no significant sensation when he did it on my right jugular, but felt pain behind my left ear when he performed this maneuver on my left jugular. In addition, when he applied the contrast on my left side I could see the contrast unable to drain through my left jugular and instead redirect back up through my ventricles in my skull and subsequently drain out the right jugular. I had a left-side styloidectomy April 2023.
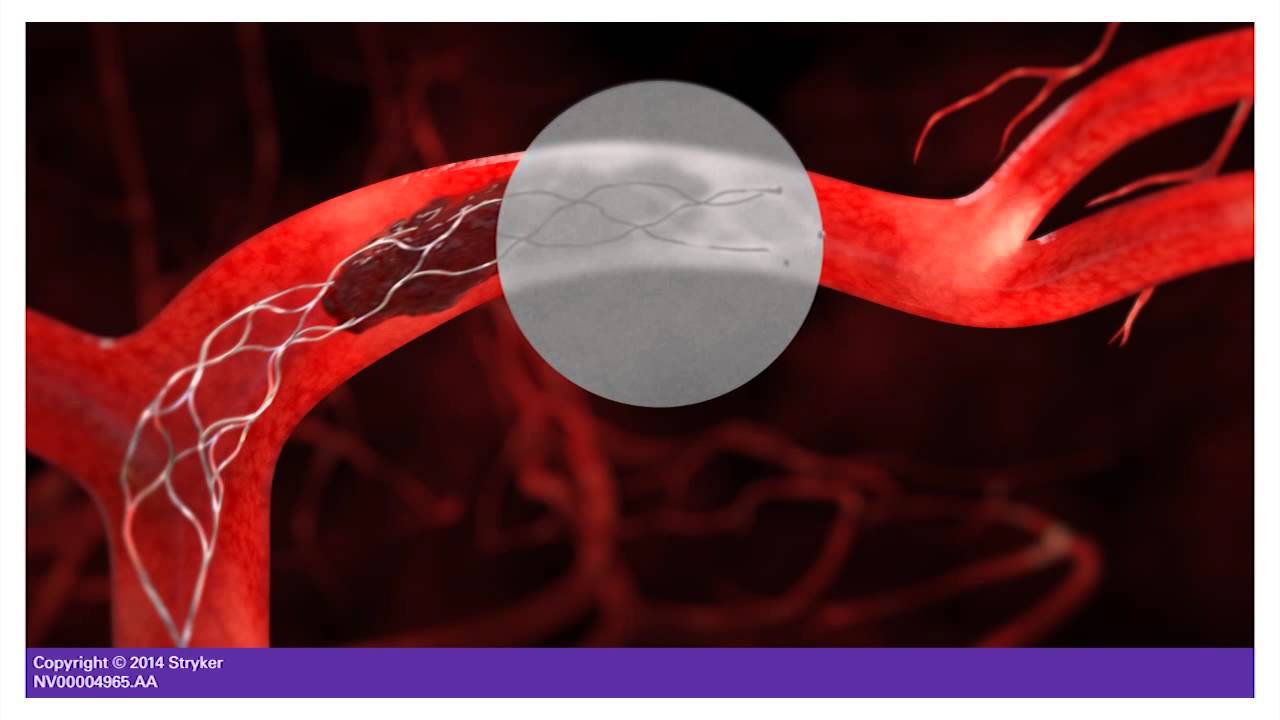
I’ve copied the conclusions from my procedure below, but in short Fargen recommended a stent be placed in the left jugular to improve the flow on the left side. I opted not to have it placed for the time being since we had the move coming up and I am still a bit weary of the long term effects of the stent. If I opted he could have placed the stent within a day or two of the scan. In addition, my symptoms overall felt slightly better while in N.C. (I resided in Denver). I let Fargen know this and he said he has had many patients who visit from high elevation states say they feel better when they come down to sea level. So that was another factor why I decided to wait on the stent, since I just moved to Houston.
I also saw Dr. Hepworth earlier this month to discuss the results of Fargen’s tests. He recommended I have a right styloidectomy and jugular decompression performed due to the high gradients recorded in the right jugular. He also recommended the surgically removing some of my SCM and/or scalenes on that side to free the jugular. I am hesitant to have a right side styloidectomy, though since most of my symptoms (aside from the head pressure, brain fog, and insomnia) has been on my left side and also because my left jugular does not seem to be draining that well after the left-side styloidectomy. Hepworth says we can test his theory about a right side fix, by seeing if a botox injection into the right SCM and scalenes temporarily resolves remaining symptoms. I will opt to get this done once we are a little more settled.
Both Fargen and Hepworth agree that the cause of my stenosis is primarily compression from my neck muscles rather than the styloid/C1 since the gradients are higher when I rotate my neck, though they both have different opinions on the solution (and of each others solution  )
)
The conclusions from my cerebral angiogram and venogram procedure with Dr. Fargen are below. I do have to say that it was extremely informational and I recommend getting the cerebral angiogram and venogram work up done by him even if you do not want a stent. Also, I really enjoyed Dr. Fargen, the time he dedicated to me during the appointments, and his scientific approach to his stenting treatment. He really is pioneering jugular vein stenting and is slowly improving the technique. I think with more time to learn the long term effects and develop best placement techniques jugular stents could be a very viable solution. He was very transparent and open about how his treatment is still considered “experimental”. I will try to upload some documents describing his practice that I received during my visit.
CONCLUSIONS:
1. Normal cerebral arteriogram without aneurysm or arteriovenous fistula.
2. There is no stenosis of the dominant, right transverse-sigmoid sinus venous outflow pathway. The left transverse-sigmoid sinus pathway is non-dominant. Venous sinus stenting is unlikely to provide benefit.
3. There is mild stenosis of the right internal jugular vein at C1 in the neutral position without an associated pressure gradient. There is no significant dilatation of suboccipital venous plexus collaterals. Provocative testing in the jugular bulb did not acutely worsen symptoms. There is severe rotational stenosis of the right internal jugular vein at C1 with leftward head rotation (2 mmHg gradient), occlusive rotational stenosis at C4-7 with rightward head rotation (14 mmHg gradient), and occlusive dynamic stenosis at C1-2 with head flexion (8 mmHg gradient).
4. There is moderate-severe stenosis of the left internal jugular vein at C1-3 in the neutral position with an 1 associated mmHg pressure gradient. There is pathological dilatation of suboccipital venous plexus collaterals. Provocative testing in the jugular bulb acutely worsened symptoms, suggesting that this stenosis may be a causative site for a component of the patient's daily symptoms. There is severe rotational stenosis of the left internal jugular vein at C1 with rightward head rotation (3 mmHg gradient), occlusive rotational stenosis at C2-7 with leftward head rotation (7 mmHg gradient), and severe dynamic stenosis at C1-4 with head flexion (5 mmHg gradient).
5. Mild elevation of central cerebral venous pressures (17 mmHg) with elevated central venous pressures (11-13 mmHg).