I was diagnosed with glossopharyngeal neuralgia sometime in mid 2023.
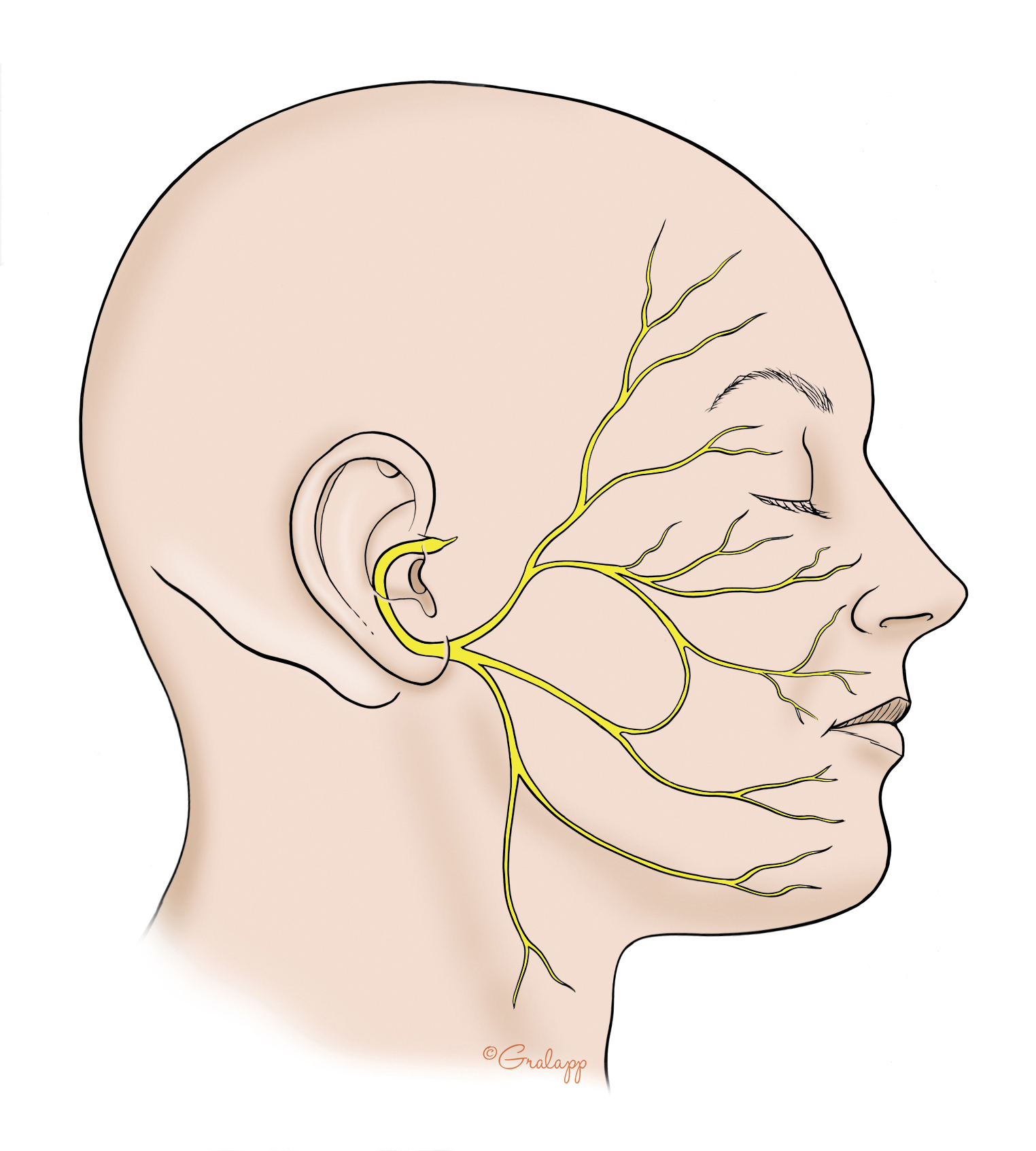
My symptoms started in August of 2022. My primary symptom is and has always been ear pain. Deep throbbing pain in the ear that sometimes changes to burning that sometimes changes to raw soreness. I visited the emergency room, and ENT, a maxillofacial surgeon who took a panoramic scan of my bite, an ENT, an audiologist, an MS- specific neurologist and was finally transferred to a neurologist who believed me when I said I had geniculate neuralgia due to the primary and exclusive ear pain.
When I requested to see a neurosurgeon, the fiesta MRI showed a clear compression of the glossopharyngeal nerve coming out of the brain stem. This neurosurgeon was Dr. Brian Jian. Together with Dr. Ballough at Kaiser, Morse in Sacramento, he performed a microvascular decompression surgery on February 28th of this year.
I had a second surgery on April 1st to remove the bone plug and titanium plate over the hole in my skull which had become infected and I was on IV antibiotics through a PICC line for 6 weeks.
I still have significant ear pain. My symptoms do not appear to have abated very much since the surgery nearly 3 and 1/2 months ago. I had a follow up MRI done last week. Shows that the the obvious nerve compression has been resolved. I requested a CT scan for eagle syndrome and found that I do, in fact, have calcified ligaments and that they are significantly longer on one side than the other (25 mm, 12 mm) They are longer on my symptomatic side.
I discussed all of this with Dr. Jian earlier this week. We are challenged with deciding whether or not to treat what continues to be glossopharyngeal neuralgia from an arterial compression or to consider my symptoms part of an ES diagnosis. The reason that we are reluctant to consider it ES is that I don’t have any other symptoms except for ear pain. I have never had throat or swallowing issues. My jugular vein is not being compressed.
He is going to do more research and ask that I join this group to chat with other members and try and find experience or research papers that show whether or not ear pain can be an exclusive symptom of ES.
I am on 1800 mg of gabapentin and 1200 mg of oxcarbazepine daily.
In an effort to have a more clear path, I have decided to begin titrating my medications to bring my symptoms to the surface so that they are more obvious. We hope that this will help us determine a more clear diagnosis.
I would be so grateful for any and all comments and questions. Thank you very much.