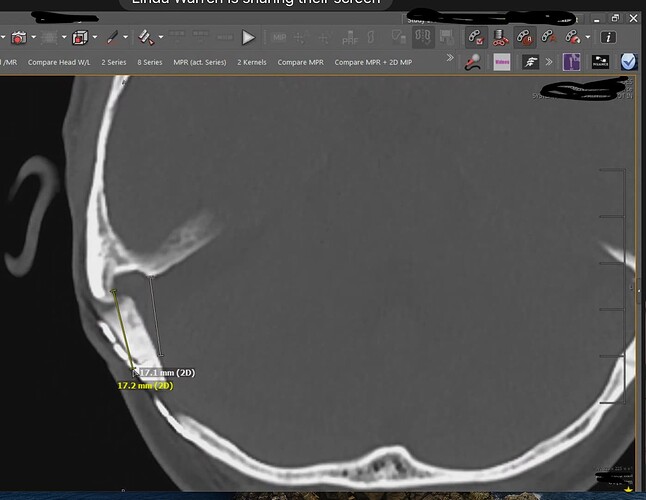
The journey for answers continues. I was combing through old CTA images and found what I thought looked like internal jugular vein compressions. Any opinions? Thanks in advance!
The left side looks compressed but the right looks ok to me to me. I’ll let those who are better versed in identifying IJV compression comment from their greater knowledge base.
I posted some images above that show possible C1 impingement on the IJVs. I’d be curious to know what @KoolDude and @boogs99 think (and anyone else who’d care to comment). Thanks in advance!
More physicians are starting to do venous stenting, but only a few have done it for a long time: Dr. Fargen, Dr. Patsalides, Dr. Amans, Dr Hui, and Dr. Pereira (Toronto). I’m sure there are other very qualified docs doing this well.
I met with Dr. Patsalides today. He clarified how he’d handle my case. He said his first and only goal for this procedure is to restore flow in the dominant venous sinus area where the clot is. Any IJV problems can be addressed later on, if needed. However, he did mention that IJV flow often improves after venous sinus stenting. He said there would be no venogram or manometry needed because, with the clot, stenting is needed to hold the vein open to improve venous flow. He said manometry is only needed to determine the need for a stent. He said it would be a several hour procedure because he has to carefully make a “tunnel” through or around the clot to restore flow.
He’s hoping the procedure won’t be necessary and the blood thinners will help dissolve the clot. However, he seemed confidant with the plan if things aren’t better in 2-3 weeks. I’m pretty comfortable with his plan, and he certainly has done enough of this stuff to know what he’s doing. He said CVST is very rare but he does about 10 of these surgeries a year, and has done around 300 of them. He also mentioned he’s one of very few physicians that tries to restore venous flow in a subacute CVST situation.
Hi @1speechpick
I 100% agree with Dr P. After all he is the authority on this and seems to have a plan to take care of sinus clot. I am sure he understands that dislodging the clot can potentially travel to the heart & lung area and could cause Pulmonary embolism so I am assuming that is why a care has to be given when placing stent in the transverse sinus (hence several hour endovascular operation). That would only be my concern regarding this procedure.
As far as IJV is concerned, I think you should not pursue this further. at least for the time being. I am not a doctor but I do not see any meaningful stenosis on both of them. Your smaller (probably hypoplastic) left IJV is slightly indented by C1. Even if you were to remove the slight C1 compression, my assumption is there will not any substantial gain in terms of outflow improvement due to its inherent narrowing and since it was not draining much to begin with. On your right dominant IJV, I do see slight compression by the C1, I am not sure if that warrants an operation since it does not appear to correlate any pre-existing IIH symptoms prior to your surgery, at least based on what you shared about your symptoms here ( not Doctor again, but my opinion here). I think it will be an issue if the compression is moderate to severe on your right dominant one which I do not see on the limited images you posted here. So I am betting that all your severe IIH symptoms are due to new narrowing induced by the surgery and you will be fine after the right transverse sinus is stented.
Thanks for your input on the images. It’s greatly appreciated!
Regarding pre-existing IIH. For 2 years prior to MVD surgery, I did have a significant history of pretty severe headaches. Dr. Hui says the headaches were from pre-existing IIH (low grade), and my neurosurgeon says they were from pre-existing trigeminal neuralgia. Truth is, only time will tell.
Dr P said he’s only had one patient develop a new clot after the surgery. They preload you with 2 different blood thinners to avoid a repeat clot. Dr. P was adamant that it’s important to wait and let the clot “solidify” so it doesn’t break off easily but still be pliable enough to make a tunnel through it (so it can be stented).
Dr. P said after we open up the dominant right venous sinus, then we will have a better idea how well the IJV and overall draining will do. And proceed with other treatment down the road, if needed.
Well, I am not here to challenge what a trained doctor had to say about your pre-existing IIH symptoms but I think you would have many more symptoms than just a headache alone (headache can have many etiologies than only IIH). IJVS is all too familiar to us that suffer from it so we have pretty good idea of the symptoms. I think you might have had mild cerebral venous congestion as Dr Hui indicated in his report but to what degree it was affecting you is not clear given the other cranial issues you have had. The narrowing of your right IJV does exist but it does not seem severe at least based on the limited images I have looked at. So the jury is out on this one. One way to find out is to address the current stenosis on your transverse/sigmoid sinuses and see if you have residual IIH symptoms, then it makes sense to pursue addressing the narrowing of your right IJV.
As usual, you are spot-on! The best plan of action is to fix the known surgically-induced, clot-based stenosis first with hopes of restoration of venous flow. Again, many thanks for weighing in on this.
I hope that things do improve without the need for surgery, but good that you have an experienced surgeon if needed. Hugs and prayers ![]()
![]()
Thank you @Jules! That is absolutely my hope, as well. I remain optimistic, despite whatever route this thing goes. I want to sincerely thank this group, @KoolDude @boogs99 @jules @Isaiah_40_31! It’s been such a blessing to have a group of people to learn from and to discuss options with along this journey. All of the surgeries we discuss in this group are very tricky and should be approached with great thought and care. Again, thank you all so much!
Things have taken yet another turn. As you all know about me, I’m a firm believer in seeking a lot of information before taking action. I recently had a head CT. I also sought a second opinion from neurinterventional radiology at NYU Langone. This doc also had the vascular neurosurgeon review the images. They decided that the bone flap from my craniotomy/MVD surgery is too far “inward” and is compressing the juncture of the transverse and sigmoid sinuses. So not only is there a clot, but they’re saying there is an external compression on the veins from the bone flap. Their recommendation is to redo the bone flap (probably lift and trim the bone) so it’s no longer compressing the veins. Since the veins have been compressed 4 months, there’s a chance the veins may not “bounce back” and down the road may still need a stent to hold things open. And, they’re saying that stenting alone won’t help because of the compression.
This would explain so many things. It would explain why, even before the CVST, I never really got all the way better, had head pressure, and other things.
Below, I’ve included a couple of pictures from the head CT that the doctor and I talked about during my appointment. I’d be so appreciative if anyone would weigh in your thoughts. @boogs99 @KoolDude @Jules @Isaiah_40_31
Thanks, in advance.
The bone flap is by the red arrow on the right (see below). Per the doctor, the venous sinus area is right next to the bone flap (blue area). You can see how much different the right looks than the left.
I did a screen shot of the doctor’s image (see below). He said the venous sinus runs through the two markings (verticall lines) on the photo.
@1speechpick - I have thought about you so much over the last months & have been meaning to check in. Humble apologies that didn’t happen before you sent this post. ![]()
I can see that the area you’ve noted is much thicker on the right than the left & what the two new doctors have said makes a lot of sense. I am sorry you’d be facing a re-do of the surgery & perhaps a stent later but if it turns your life around, it would be so worthwhile!
Did they happen to say how the clot would be managed? You sure wouldn’t want that to escape & lodge someplace else & cause yet another problem. Perhaps just getting the pressure off the transverse & sigmoid sinuses would allow it to break down & dissipate?
You are an amazing self-advocate & it’s paying off for you in providing you with answers that sound like they’ll be very helpful in resolving your symptoms, even though the journey has been prolonged. It sounds like you’re feeling more optimistic which is good, too. This has been such a rough ride for you.
I will pray for you to make the best possible decisions about upcoming treatment & by whom. ![]()
![]()
![]()
Thank you so much! The doctors I talked to today didn’t seem to think there would be a problem with the clot. They’re not going to directly do anything with the clot at this time. I will remain on blood thinners for a while. The surgery will be very surface with trimming and lifting the bone.
So this next surgery won’t be invasive like the first one? It does seem to be a more superficial (as in not deep in the skull) problem. That means an easier & hopefully quicker recovery. I’m really glad to know that. ![]()
So sorry that you’ve got this issue, but pleased for you that the doctors seem to have found out what’s going on. I’ll join in with @Isaiah_40_31 in praying for you & for wisdom. Hugs as well ![]()
![]()
All I can say is WOW. One would think that aligning the bone back in it’s proper place would have been the easy part of MVD surgery. And was this visible on your CT from a month ago?
I’m glad you are getting to the bottom of this.
@boogs99, thanks for your reply! I guess the only upside to having a lot of imaging is it leaves an evidence trail.
Below is the CT image that was done right after my MVD surgery. To me, the enlarged bone flap is pretty obvious but it seems to me like the bone may perhaps have grown a little inward (when comparing this image to the 10/2/22 image). Let me know your thoughts. Thanks!
It does seem a little bit more pronounced in your more recent image. In such tight quarters very small size differences can cause very large problems.
I agree. Per Dr. Raz (NYUL NIR), the flap was placed “too inward”. But to me it does look like the bone grew even more inward. Unless it’s just the difference in the points of the axial images.
Regardless, it looks excessively thick compared to the other side.
@1speechpick first I am really sorry to hear that a new bone compression was induced by the surgery. My knowledge in this area is limited but I guess you have no choice but to decompress the sigmoid/transverse sinuses if any future stent is to work to open the sinuses up. I hope re-opening the healing wound would not induce additional symptoms (Tell them to be careful this time). I would ask them to carefully examine the bone graft as some areas appear thin and can potentially cause CSF leak if pressure builds up in brain. Also, I hope they re-examine the whole operated area for any potential leftover fluid to make sure it clean and healing properly. So I can only offer my sympathy and wish the repair work goes smoothly for you.