@KoolDude, thanks for your response. I think the bone flap revision is a pretty easy surgery, comparatively. I’d rather have my local team do it, but that probably doesn’t make much sense if they didn’t get it right the first time. I’m scared going to an unknown, yet they’re the only ones that found this compression. Or even looked hard enough to find it. Can you mark in the image where you think the bone graft is pretty thin, please? Thanks!
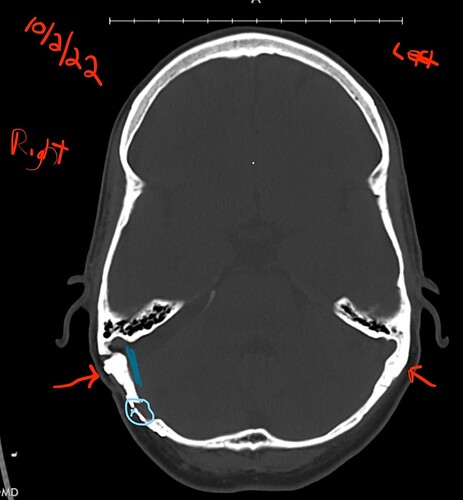
I really do not know if this is an artifact of the imaging but the area (Cyan circle & tiny arrow) point to an area which appears to be thinned compared to the contralateral side. Based on some research, MVD can also cause post-surgery CSF leaks. So it won’t hurt to bring it to their attention since they are going to be drilling the bone.
Funny how it’s too thick in some areas and too thin in other areas.
@1speechpick Your story is inspirational. As someone with severe gastroparesis, I wanted to ask if your gastroparesis immediately resolved after the initial MVD surgery?
Can you describe your gastroparesis? Did you have low acid? Or excessive stomach acid production?
@Bowser my husband is awaiting a consult with Dr. Kamran (and a couple in the US). I know Dr. Kamran did your recent procedure.
JC was previously diagnosed with gastroparesis. Originally he was put on metoclopramide but that med comes with a host of side effects, including neurological. Then he had Domperidone, which was much better. Domperidone is not available in all countries (including the US) but it is here in Canada. I did a quick Google search and I believe it might also be available in India.
He had 2 scopes and was put on a PPI. Over time, the PPI caused side effects. It turns out he had low acid! So he slowly slowly started added digestive enzymes and acid into his diet. It took about 6 months (maybe more), but he got off the PPI and Domperidone. Now he can have meals without the extra acid but he still goes through points where it feels like he can’t digest and he goes back on them for short periods of time. He’s been on a soft food diet for ~2 years because of digestive issues combined with TMJ and what we now know is Eagle syndrome.
The combination he takes is Betaine HCL Pepsin, Digestive Enzymes, and something called Bile Force which is bile salts, triacyglycerol and pancreatic enzymes.
The surgery sounded so promising to start, and it’s disheartening to hear about this turn of events. I wish you all the best in the coming weeks/months and that this part of your recovery is behind you.
@1speechpick Was the original MVD surgery done only on the right side, the same side where the CVST occurred?
Yes, my CVST occurred pretty much at the surgical entry site of my MVD surgery on the right side. I clotted in the transverse sinus, sigmoid sinus, and the jugular bulb.
Thanks for your kind words. And no, my gastroparesis (GP) was not immediately resolved after my MVD surgery. It took a lot of time, and also had other significant contributory medical factors. My gastroparesis was diagnosed by Ohio State GI motility specialist via gastric emptying study (GES). I had craniotomy/MVD surgery to address arterial compressions diagnosed via Fiesta MRI involving the trigemenal, glossopharyngeal, vagus, and accessory cranial nerves. My gastroparesis was pretty severe. I lost 50 pounds (weighed 102 lbs), had daily nausea and vomiting, and ended up with a feeding tube for 2.5 years. For 2.5 years my nutrition consisted of 50% oral feeds (liquid diet only) and 50% tube feeds. All tube feeds went into the small intestine because my stomach (gastric body) had all but stopped processing food. I definitely had high acid. Again, my gastroparesis was multifactorial. I hope that helps. Please feel free to ask any questions!
Oh okay! That sounds incredibly challenging! Are you able to eat normally now?
YES!!! I eat normally and now weigh more than I ever have. Gastroparesis continues to improve gradually. I’m incredibly blessed!
Fantastic!!
I haven’t been on the forum much lately. So, if there’s anything I can do to help, please let me know!
So this answers an important question. Whether you are looking at Eagle syndrome or MVD surgery or whatever else, a Fiesta MRI can tell you about those nerves looking for a differential diagnosis. Not sure if a Fiesta-C/3d Ciss is better. Seems like some studies say yes.
Also, not sure if it can tell you about other things not involving need for MVD
I’ve reached out to OSU to potentially video consult with your surgeon (Dr John McGregor) and have him look at my FIESTA or 3D CISS MRI. Meanwhile @KoolDude is also taking a look at it!
Here it is: https://www.dicomlibrary.com/?study=1.3.6.1.4.1.44316.6.102.1.20241026202342600.18529912117662337003
He may not be able to video consult. Dr Old at OSU who does Eagle Syndrome cant video . At least for first visit…
That’s correct. That is true of most of OSU’s physicians. Most OSU physicians require the initial visit to be onsite, and subsequent follow-ups can be virtual if you live within the state of Ohio. I’m unsure if virtual follow-up visits can be done across the state line, in the post-covid era.
Dr. John McGregor at Ohio State Wexner Medical Center diagnosed my trigeminal neuralgia (and other cranial compressions) and did my MVD surgery on 6/14/2022 to fix my cranial compressions. I had major post-op complications, none of which were his fault! I had post-op CVST (blood clots in the transverse sinus, sigmoid sinus, and jugular bulb…on the surgery side). The clots caused secondary intracranial hypertension. Dr. McGregor placed a lumbar shunt to relieve the intracranial hypertension. Unfortunately, the lumbar shunt placement caused a major lumbar CSF leak (had to go to Duke to have it diagnosed). After multiple failed blood-patch attempts, OSU did the CSF leak repair (required 2 laminectomies and vp-shunt placement). However, the leak repair and vp-shunt placement were not done by Dr. McGregor; he handed my case over to one of his colleagues. The surgeries were completed by Dr. Xu at Ohio State. Dr. McGregor retired in June of 2023 and took a few months off. After some time off, Dr. McGregor returned to OSU part-time but in a little bit different capacity (I think). There’s been a bit of staff shuffling at OSU. I don’t think he’s doing the intensive MVD surgeries or managing shunt patients, as he’s no longer my neurosurgeon. I think he’s now managing surgical cancer patients. If you do get to see him, he’s brilliant and so very kind…and I’d highly recommend him! I had complications that no one could have predicted. As a result of his original surgery…my trigeminal neuralgia is GONE! I no longer have the daily horrible headaches or facial pain.
I so glad for you @1speechpick that the TN has finally gone, & that your gastric issues are gradually improving…you have had such a long journey to get back to health! I hope others will read this & keep the hope that although it seems really grim things can improve, & thank you so much for coming back to update us & help others ![]()
Your story is inspirational, @1speechpick. I’m so glad your doctors were able to refer you to others who could fix the things they weren’t able to & that, with persistence & time, you were able to achieve the level of recovery you have. Jules & I prayed for you & probably some others, too, & God has answered in a most marvelous way!
I also thank you for coming back to share your journey & victorious outcome. ![]()
Thank you so incredibly much! There are so many incredibly kind and caring people on this forum! I plan to participate on this forum more. You all were here for my when I was at my lowest of lows. The least I can do is share my story in a way that will help others. Blessings to you!