I have been battling daily pain for 3+ years now, and I honestly no longer know where to turn. I dismissed ES about a year or two ago, because it was considered quite rare and because I did not match most common symptoms listed.
But now I’m not so sure, so here’s a very abbreviated history:
- My issues started in 2022 on upper left, but in retrospect I think I’ve had minor issues for more than a decade.
- I had symptoms in my ear and in my teeth and, since I only had few teeth on my left side, over time I removed all 3 of them (as each got fully inflamed, one after another).
- I’m currently left with just front two teeth there and I eat with removable prosthetics. TBH I’d be happy even as a dental cripple if there was no pain, but the issues did not stop there.
- My ear (and part of my cheek) remained highly sensitive to cold air drafts.
- I originally thought I had Trigeminal Neuralgia (another rare condition), so I did several head and neck MRIs. These did not reveal any compression of the trigeminal nerve.
- I then thought I had acquired (or already had) TMJ disorder (esp. with pulling teeth, despite not really having most of teeth there for decades), so I went to a TMJ specialist here in Houston, did the Jaw MRIs and examinations (even Botox injection), but nothing untoward was revealed.
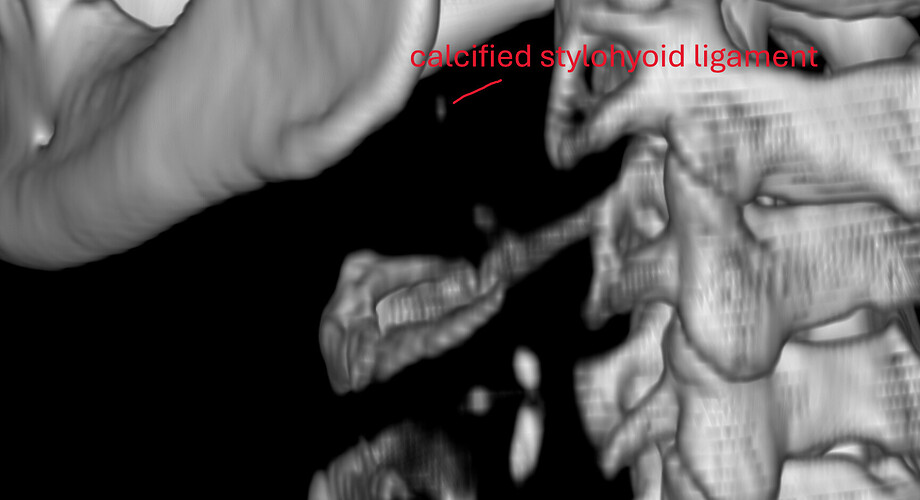
- Finally, my oral surgeon spotted something on the dental CBCT and asked me to check if I have ES. So, I did the CT for ES and it revealed a calcified portion of the stylohyoid ligament.
And, before we proceed, I literally looked at the 3D rendered CT today, and the calcified portion is only ~15mm, detached from styloid process, and about 1.5mm from C1. In the CT results, it says “partially calcified stylohyoid ligament, combined length 31mm” but the keyword there is “combined.”
Now that we cleared the history and current state, here are my symptoms:
Skin and Superficial Muscles
(most of my symptoms are manifesting here, so this is the longest section)
(1), (3), (4), (6) are “always” symptoms. I have them all the time. So, dull pain in blue area, sensitivity to cold drafts in green areas, yellow tender areas (pain on pressure or massage), and neck pain (pink area) are always present.
Neck pain (6) gets worse with turning head to the left, and even worse if head is then tilted. It is also worse if head is just tilted to the left.
(2) red area pain shows up when things worsen from one of the above, or some other factor. E.g., I got cold air draft, or I massaged the (1) or (4) instinctively, or I tilted my head to the left for too long, or I drank/ate some stimulant (caffeine, or too much sugar in a meal), or stress, or I used cheek muscles too much (like keeping a smile for too long). I can always cause and/or increase (2) pain by either hunching over something or by tucking my chin in and tilting head left, or by leaning on my left shoulder while sitting/lying down.
Normally, jaw movement and speech is not that much of an irritant, but once already (2) is irritated, moving the jaw makes it worse (speech or otherwise).
(5) will show up once the other symptoms are really bad. Then, my tooth will feel inflamed. Basically, neuropathic itch pain. Hard to describe. This is not that often, I actually had a “pause” of this for about 2 years. Came back in the last month.
There is also sometimes a dull pain traveling down my throat and into the chest. Feels like it follows the path of the jugular. This is not always present.
Hyoid Bone
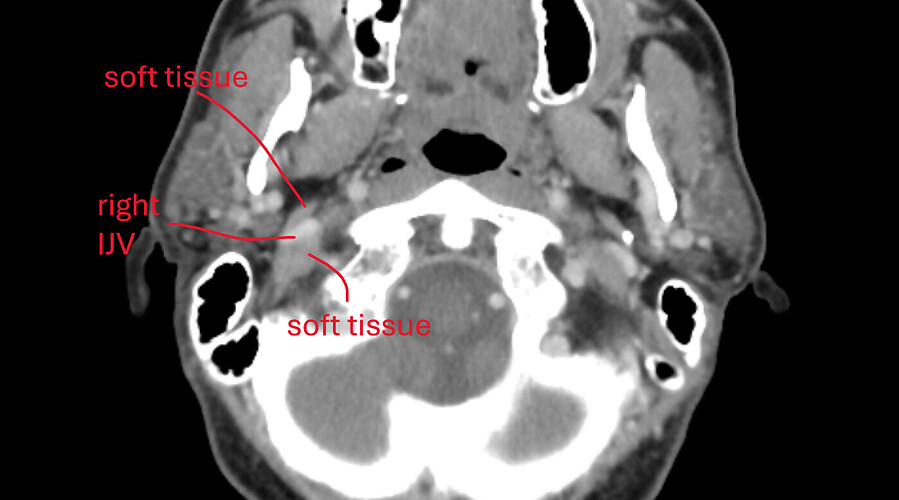
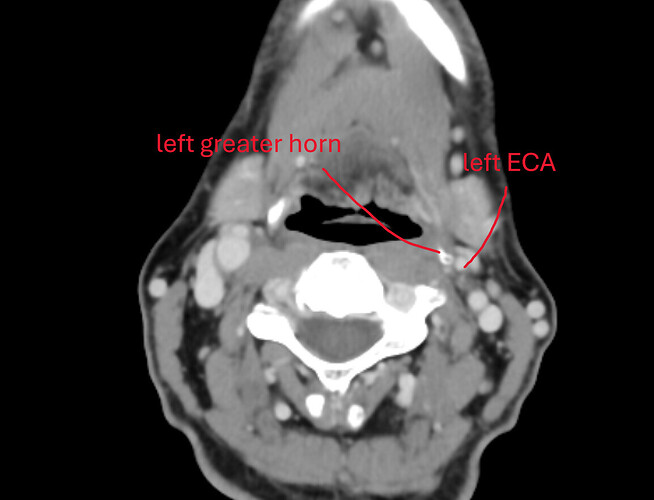
It is quite lop-sided. Left side is quite low, right side is up. Not sure if that matters, but mentioning here. Pictures, below, will show this.
Mouth and Throat
Inside the mouth, there is same dull pain all the way to the back, at the throat. Left side. There is a muscle or something there on the side, which one can even press a finger against (if your gag reflex is low) and feel it tense up when swallowing. That area has dull pain, sometimes burning.
My tongue sometimes feels like it got scraped by something hard (left side only). I’m not sure if it is a burn, but it feels kind of like one. Like spicy food made it back there a bit. This symptom is more recent, last few months.
Sinus
Inside my nose, left sinus is often swollen shut if I sleep to the left or if my head is turned to the left when I sleep. It is also always more obstructed. There is always some drainage on that side, as well.
Additional Symptoms
- Ear ringing. Always. Feels like it is more from the left, but both ears ring. Gets worse as my other symptoms get worse. Especially if the cold air draft irritates the ear canal.
- Hearing is off. This is only sometimes. When it happens, I feel like there is something blocking my hearing on the left, like someone slapped me on my ear and I cannot hear properly afterwards. Or like the ear pressure is wrong. I checked (with otoscopic camera), there is no obstruction in that ear.
- Cannot tell you with 100% certainty whether swallowing generally feels odd on the left, because of too many other symptoms always present. I think it does feel a bit weird on the left, but I may have gotten so used to it over the years that it is not easy to notice. I don’t think it is painful, but it is slightly “off.”
- Normal use of jaw (speech, eating) does not cause issues unless I’m already in “cheek burning” phase (bad symptoms), but opening really wide (like for yawn) will hurt on the left first time, then a bit less in subsequent tries.
- I will sometimes get a headache from all the pain.
- I will sometimes feel unwell. It will start with sudden sweating and can last up to few hours. I have always attributed it to some involuntary panic attacks and anxiety.
- Rarely, there is a feeling of tickle in my throat on the left. Like when you are sick and need to cough. Basically, I tear up and I need to “cough it out” at that point. But, there is nothing there, it is just a tickle out of nowhere.
Additional Data
- I already had my tonsils removed as a kid.
- Full disclosure, I also have sciatic pain in my left leg. Comes and goes, mostly mild. The symptoms there can get worse if my facial and neck pain symptoms get worse. Almost like I get “sensitized.”
Mental State
It is bad. I am very much hopeless. I don’t fit anything clearly, not TN, not TMJd, not ES (based on my reading of these forums), not MS (multiple sclerosis). Just “pain of unknown origin” which is the worst thing, because diagnosis is half the battle. Without a diagnosis, a person is lost in symptoms and no specific targeted treatment.
Last year I was losing 10 lb / month from pure depression. Yes, I was suicidal. I climbed out of that when I removed my teeth and my symptoms started improving, but in recent months I’ve acquired additional symptoms I did not have before (like the throat burning thing). I don’t want to fall back into those thoughts again ![]() .
.
I’m afraid to travel anywhere. I am afraid of air! I know, it’s insane, but I’ve been hit by drafts of air in airports, outside, in hotels, and if I don’t escape the draft within minutes, I will be in Hell for the next 24hrs. I sleep in a cubby to prevent air movement around my head.
I cannot sleep on my left. At all. This has caused me issues with my right shoulder, so I’m kind of stuck on my back at this time.
CT Pictures
Sagittal view. Calcified portion of stylohyoid ligament. There is a little bit more in another slice, but this is the most of it.
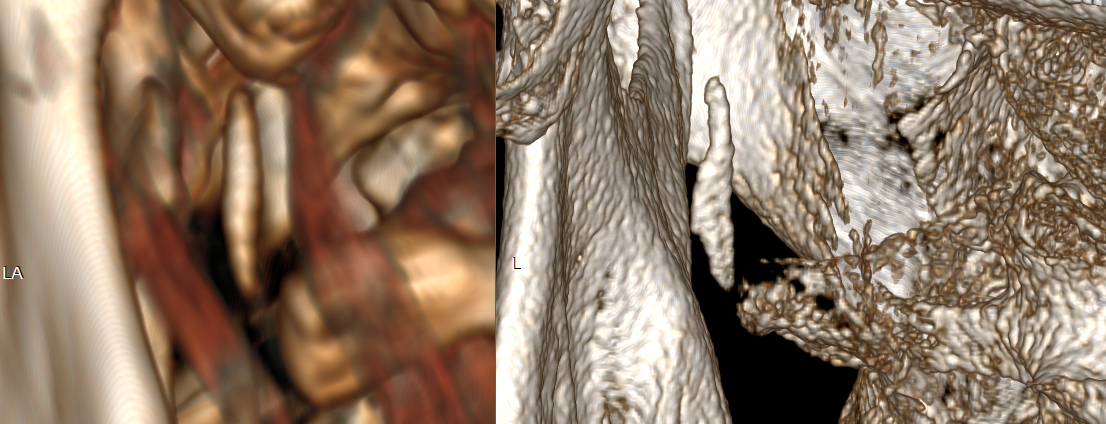
3D views – one is low-res from above CT, and another is high-res from a CT with 0.2mm slices (most detailed CT I’ve ever seen). Distance from C1 is measured at about 1.5mm, length of calcified portion is ~15mm and it is flatter on one side in the lower section, with a “bit” sticking out slightly.
An animated gif with hyoid bone. Note the horns, left is quite lower than right.

I am also including some animated gifs of axial, sagittal, and coronal views of the calcification from the last CT scan.