@GCD once again, I can’t begin to express how helpful you have been. Regarding my twins, they are 26 and living the life in Nash Vegas! As everyone says it goes extremely fast, but I loved all the ages, especially the young ones, And looks like soon you’ll be on the other side of surgery and on the road to recovery and be able to enjoy your life and children to the fullest.
Thank you for the information regarding alternative drains… Did not know and it’s quite helpful. We do not know why I was passing out, my internist suggested it was a vasovagal response to the pain… But with more I’m learning perhaps it was a compression of the vagus nerve that took me out and woke me back up. I have very specifically not put my head in that position since, so at least I am trying to protect the nerves from all this irritation.
So another little interesting piece, which I am only thinking might’ve been the catalyst for this acute reaction I’ve had, is that we were going out of town to a function and I was in a lot of pain so I used my tens unit for too long and too high. I had not used it in several years but have used it with this intensity in the past without a problem. Trying to connect dots, because I have no other reason why this happened… But is plausible to me that I irritated quite a few things with the tens unit, it was not on my neck, but it was on my shoulders. (Saw one post where someone mentioned they couldn’t handle vibrations. And that made total sense is if my everything was inflamed, and the styloid was in there, just bumping around like a pinball machine, it’s set off a reaction all over the place). And of course, this is my speculation, because no one else has any better understanding, as we have all seem to find out.
I knew the next morning that my muscles were unhappy, (the top at C1 and one is at the bottom C7). I layed down for a nap, my trapezius muscle went into a ridiculous spasm, which pulled my left shoulder up towards my left C1, and then I blacked out. The same thing happened a week later in the same position.
So while I’ve been chasing this (one sided) cervical pain for years (with no one understanding why I have no issues on my right side), this put me into a whole other level, and I’ve been in a very acute phase since that event six weeks ago.
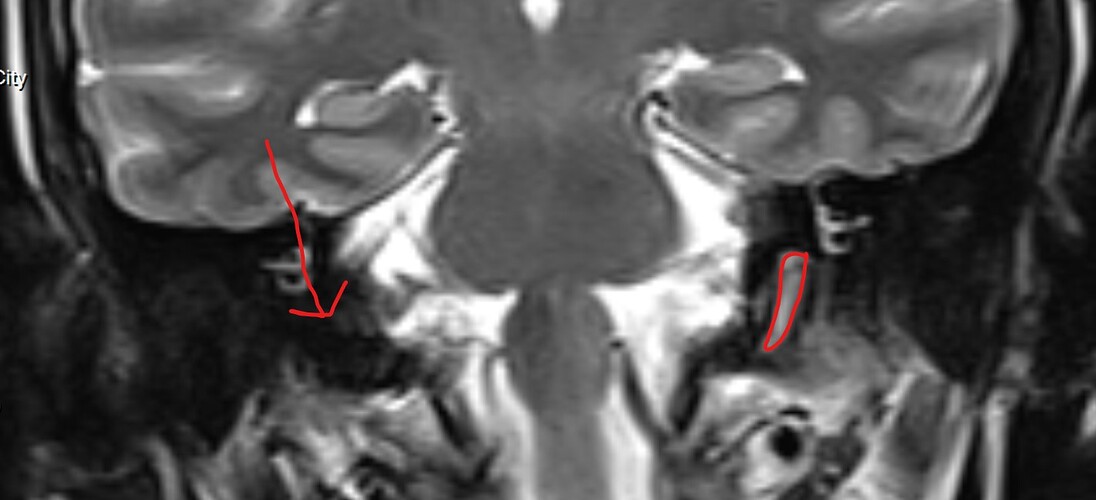
I have been aware of my C1 and its proximity to the arteries and always concerned about compression… But never heard of a styloid until a week plus ago. Want to friend who’s an oral surgeon for Botox in my TMJ and temporalis muscle, and he did that panoramic x-ray that you were mentioning, which is where this was identified.
More than you ever wanted to know…. quite interesting that everyone has had to figure this out for the most part by themselves.