I wrote this for my FB page as tone will show (really for me as it pops up as a future memory…), but wanted to share here as well in the event that anyone gets anything out of it. i will say this. After the added findings of Dr Fargan, whether or not they are causing symptoms, I am very glad that I did not dive head first into surgery with Dr Hepworth (which was right away recommended). If there is one bit of advice I would give, even if you’re seeing someone who is considered at the top of the game, go and see another one as well (if you can. i know we don’t all have that luxury).
And I will add that I mean this especially if you are a VES vs ES case.
Tomorrow is a big day
Not because big things will change but because big information will be revealed.
Jesper and I arrived in North Carolina on Thursday. We are staying at the SECU house, a true gift of a place (more on that later).
We came here for our appointments with Dr Kyle Fargen, a ground-breaking cerebrovascular neurosurgeon. We had a 2hr consult with him on Friday (I was blown away that over 60 minutes of that time was actually with him!).
When he walked in the room he had reviewed all of my relevant imaging. He understands our patient population and told me to please lie down on the table for our discussion if it would be better for me (heaven opened up and just about swallowed me then).
And so for the first time since early 2019 I had an appointment with someone with serious discussion and concentration without my head exploding, my brain wigging out (more than current baseline) and being unable to even seethe questions that I had on my paper.
We are here for Dr Fargn to do the catheter angio/venogram and then a lumbar puncture. In the first he will wire a line up via the femoral artery in the groin area into my head. I will be awake and strapped down to the table a-la Frankenstein mode.
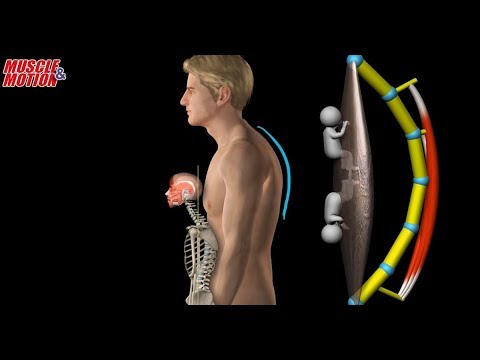
He will do two things. First he will be taking pressure measurements. If the flow of blood differs in rate, slower above and then faster below, that represents an undesirable impact. So he will measure in the head , the jugulars, and the veins blow as blood gets pushed back to the heart.
Next, he will take provocative measures, specifically in the jugulars. Here he will have me turn my head one way, then the other, and then they will lift it to try and mimic looking down. In those positions he will push fluid hard to see what if any symptoms are recreated. In someone that is asymptomatic, they will hear a wooshing sound. While someone who is severely symptomatic may contort from the sudden pain or dizziness or whatever
None of these will be the same as being upright as your head is fully supported and thus muscles relaxed on the table. But in taking these measures one can extrapolate how natural movement impacts the jugular vein and thus the flow of blood, and importantly if these are actually contributing to your symptoms. I of course want to have my symptoms get nutty because that means we have something that we might (might!) be able to fix.
On Friday he said that my situation is potentially complex as certain things stand out in the CTA/V scan that was done
- Transverse sinuses both have arachnoid granulation that might contribute to flow issues – he suspects this is a red hearing but needs to be looked at
- There is the jugular narrowing at styloid and C1
- The Left jugular is narrowed lower as well from the carotid artery and muscular compression (and this scan is was lying flat, so that’s muscles at ease rather than all tense)
- And the one that is apparently exceptionally rare and may be a doozy if it is contributing to symptoms, my brachiocephalic vein in the chest behind the sternum looks really tight and flat. (quick anatomy class: The left subclavian vein comes over, joins up with your left jugular vein becoming the L brachial cephalic vein which travels for a distance behind your sternum over to the superior vena cava that dumps everying into your very own recycling container, the heart. The vein right there (behind sternum) is very narrowed
- Finally after this is done he does the LP to remove fluid, lowering the opening pressure, and see if you feel better from that
Depending on what he finds, he will make his recommendation for what, if any, surgery I would need:
- I’m not sure what he would do if we find the granulations are an issue, but he may think a stent is an option to move more blood to the right side.
- This is the one I was expecting to be the issue and expecting him to have a no brainer response that I need a left styloidectomy and jugular decompression as Dr Hepworth (ground breaking peer) is recommending. Dr Fargen points out that it is common for patients who have this surgery on one side to then need it on the other because symptoms commonly increase there (I read this a lot on our group page!) and for them to go on and need a stent as the vein just can’t keep itself open (I read this a lot too – it’s common to read of someone’s improvement and then some time later they post again that their symptoms have all returned and they don’t know why…
- This one is tricky and not a good finding. That unlike the other veins in the head which have great support and strength in them to stay open, the jugulars are like the veins on the back of your hands. If you push on them at all they flatten, impacting flow. So where at the top you can remove the styloid (and potentially shave a bit of C1 if that is insufficient), you can’t remove the carotid artery and necessary muscles. It this is an issue, then it may require stenting. But stenting is no longer done by these Drs unless styloidecomy has failed to provide sufficient relief of the vein recollapse (happens a fair bit). The stenting that would be involved here is also highly experimental, with a small stent placed at the top and a larger one, flush below the small one, so that the entire jugular is stented. But there have been complications that have resulted in a couple of deaths from stenting the jugular, and the more likely other complications involve life long nerve impacts and pain from the stent itself. So we don’t want this.
- Number 4 is the worst possible scenario. If this is a source of pain/dizziness etc then we’re in trouble. The flattening is because it’s being pushed against my sternum, which I need…. And the only thing that can be done is to break open my rib cage and rebuild it, giving the vein more space. This section is long, a copy paste from my notes so that I have it here when I lose them

o “The reason that’s problematic is that that impacts flow out of both your arm and your jugular. Patients who seem to have that problem tend to have predominantly left sided jugular symptoms and much larger component and arm symptoms on the left.
So when we go in we measure pressures and often what we see is we’ll see stagnating contrast much worse than the right because there’s an outflow problem down here
o Importantly if that’s a major problem styloidectomy won’t do much for you
o There are people who will collaterize to the other side… we’ll see the blood go to collateral veins and a lot of that cross over to the right and then down the jugular vein on the right side where the flow is not as impaired.
o There’s not a way to fix that without taking your chest apart and reconstructing your chest to make room. I know of one person, a cardiothoracic surgeon in Johns Hopkins who did that and they reported improvement in symptoms, but this was just a month or so ago and I don’t know how the patient is doing now… He also shared that he had seen (or maybe even done himself) a stent placed to open it up, but the stent got ruined in no time because the pumping thrashes the stent against the sternum which wins…” - Finally, I don’t remember what we do if it’s number 5. I think he expects this not to be an issue. But a drug like diamox at the least… perhaps a shunt?
He suggested that my left sided TOS symptoms could actually have been misdiagnosed and it being the brachiocephalic thing. But as I ponder it, the fact that the left symptoms in my forearm and hand are almost identical to those on the right, I’m banking on this NOT being the case.
So, let me add here, that I am not buying into number 4 being a major issue and therefore am pretty chilled out about it all.
I am super crazy excited to have this procedure done and can’t wait to hear what Dr Fargen shares with us after
Wish us luck ![]()