Hello everyone,
I’ve posted before, but not in a few years. I have a very long history of chronic pain in my head and neck. I had Eagle Syndrome surgery a number of years ago (bilateral styloidectomy) and it didn’t help that much. I highly suspected vascular involvement at the time, but the doctors didn’t pay attention to these possible complications.
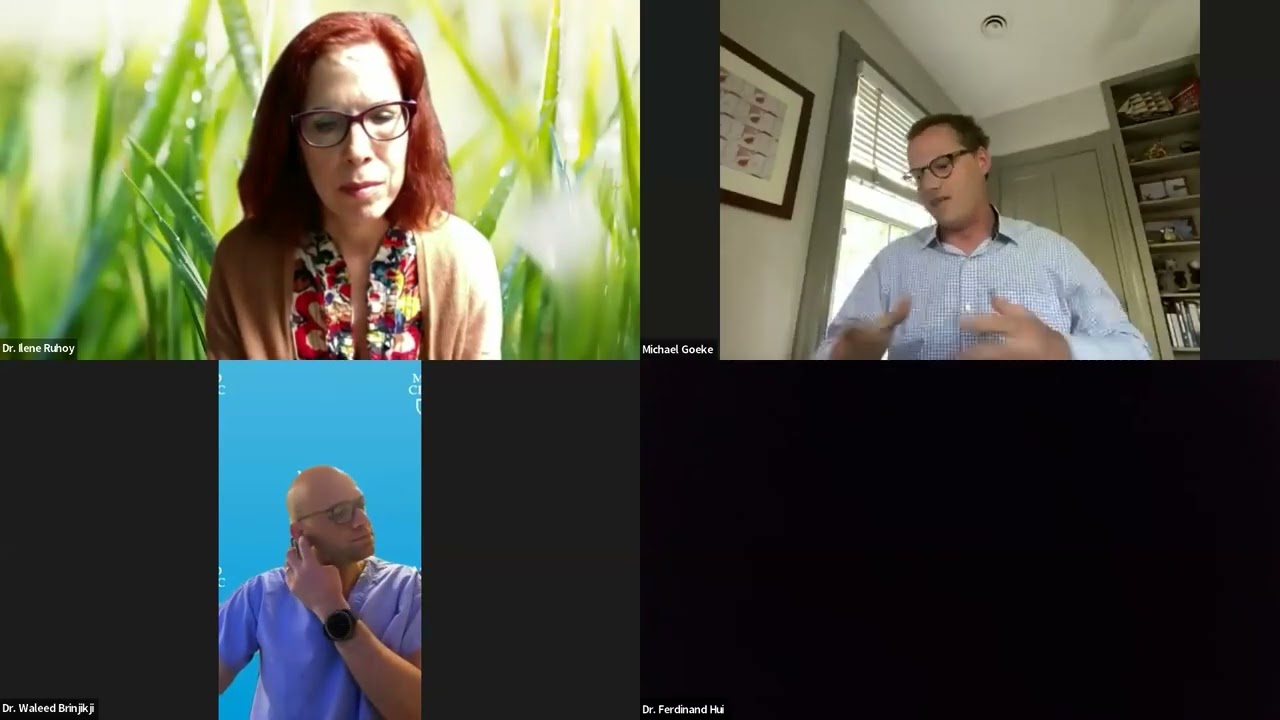
I recently saw this video on YouTube and it really put a lot of things together for me:
Basically, I am convinced that I have jugular vein stenosis, leading to intracranial hypertension and a possible CSF leak.
I’ve also learned much more about the role of the upper cervical vertebrae, especially the transverse processes of C1, in causing compression. I think C1 is probably my primary mechanism of compression, rather than the styloids. This would explain why I didn’t improve more after my styloid surgery.
I’m going to try to get an appointment with Dr Hepworth in Colorado, who I understand is one of the best specialists on the vascular type of Eagle Syndrome. Two questions:
- Is he booked out a long way? How long does it typically take to get an evaluation and all relevant testing to diagnose the problem?
- And then, how long does it typically take to actually schedule surgery (if necessary)?
Does anyone know what his typical procedure is for evaluating venous congestion, intracranial hypertension, CSF-leak and other complications of Eagle Syndrome and C1 impingement?
I have an appointment with a neurologist this week, but I don’t know if they’ll have relevant experience or be much help in getting closer to a diagnosis.
I do have some other ideas:
- I know the potential role of prolotherapy in the treatment of Eagle Syndrome has been discussed on these forums. In my mind, it seems to have less of a role in treating the stylohyoid ligament itself, especially if there is vascular compression.
However, my current hypothesis is that the primary mechanism of compression is a forward shifted C1 vertebrae (and possibly C2 as well) due to craniocervical instability. I do have some chronic back issues and I feel that spinal alignment played a role in the development of this disease, as well as a role in treating it.
If I’m correct, then it would seem that prolotherapy, PRP, even stem cells could be very helpful in strengthening the ligaments around C1, C2 and the rest of my cervical vertebrae, pulling them back into alignment and creating more space for the jugular vein to drain the head. Any thoughts?
- I also have an appointment with a local chiropractor who does nonsurgical spinal decompression using a machine called the DRX9000:
I had MRIs of my entire spine and there are some areas with disc problems, in both my lumbar spine and my cervical spine.
I feel like decompression of these discs may improve my overall spinal health, improve the normal curvature of both my lumbar and cervical region, and help my C1 and C2 vertebrae move back into normal position, improving venous drainage from my head.
I do think these two therapies could be very supportive of my recovery, but the main concern right now is having a full assessment of my jugular veins, and intercranial hypertension.
The reasons I now suspect a CSF leak are:
- Clear fluid coming out of my nose with no other cause. I’ve ruled out infections or allergies.
- Post-nasal drip
- Metallic taste in my mouth
- Severe headaches, though these could have other causes
Is it correct to say that it would not make sense to repair a CSF leak if it is caused by venous congestion from jugular vein narrowing? Meaning, I should have the venous congestion fixed, and then repair the CSF leak if necessary?
My last question, is it helpful for patients with venous congestion due to Eagle Syndrome to be prescribed blood thinners? I think I recall hearing that Dr Hepworth prescribes them. I’m absolutely desperate for relief and I’m willing to try anything at this point.
I know that’s a lot of questions. I really appreciate this forum and everyone’s support.
It seems to me that the venous implications of this condition are beginning to be more widely understood, which means I may finally get the help I need. I can’t tell you how many doctors I’ve seen for this condition in the past who had absolutely no understanding of the venous drainage implications of this disease. They did no workup or imaging for the veins at all.
Thanks again.