My most recent ENT in Toulouse has no experience with what I believe is my jugular ES. I am reluctant to undergo surgery with her, although she is very nice and knowledgeable, because we still haven’t determined which side has more of a compression. Despite 2 CT angiographies showing no evidence of NO jugular flow on the left side, the ultrasound she ordered DID show blood flow on the left side, but not as much. I do not know, and I don’t think this Dr. knows, how to determine if the flow is sufficient. Is there a standard for ‘sufficient blood flow’?
The ultrasound doctor said she could not tell if there was a compression even when I had my head in different positions–so there was no obvious shut off of the blood flow. I don’t understand it. The styloid on the right is longer and curved and my symptoms are all on the right. My ENT thinks to remove the left styloid to help more blood flow on the lefts side since there may be pressure on the right (it looks enlarged) but that eventually both will need to be removed. I don’t want a wasted surgery so I need another opinion. I’d rather have both removed at the same time to get it over with but this dr. says ‘in case something goes wrong on one side’ I should only do one at a time. That doesn’t give me confidence. Also, she says the styloid will continue to grow and thicken over time. Is that true? If it gets thicker, that will be a problem. Can’t imagine it will get longer. They are already 4.6 cm or so.
I can’t answer your question about how sufficient IJV blood flow is determined, however, I will comment on the “in case something goes wrong…” statement. Even when a bilateral surgery is planned, the surgeon always has the option of making it unilateral if (s)he feels the initial styloidectomy didn’t go well or the patient is not tolerating surgery well.
It is important to see a surgeon who is experienced w/ bilateral styloidectomies, though, & especially one who will do your external incisions high enough (under/behind the ear) so the carotid sheath/IJV can be seen & IJV blood flow assessed after styloid removal. A discreet incision lower in the neck will not allow for assessment of IJV function & removal of styloid to skull base can only be assumed to be relieving IJV compression when C-1 could be the greater source of compression.
Styloids when left in an elongated state have been known to continue to grow & in some cases thicken. We had a member here who’s styloids measured 8+ cm at the time of removal. I would assume the size of a person & length of neck might determine maximum styloid length though.
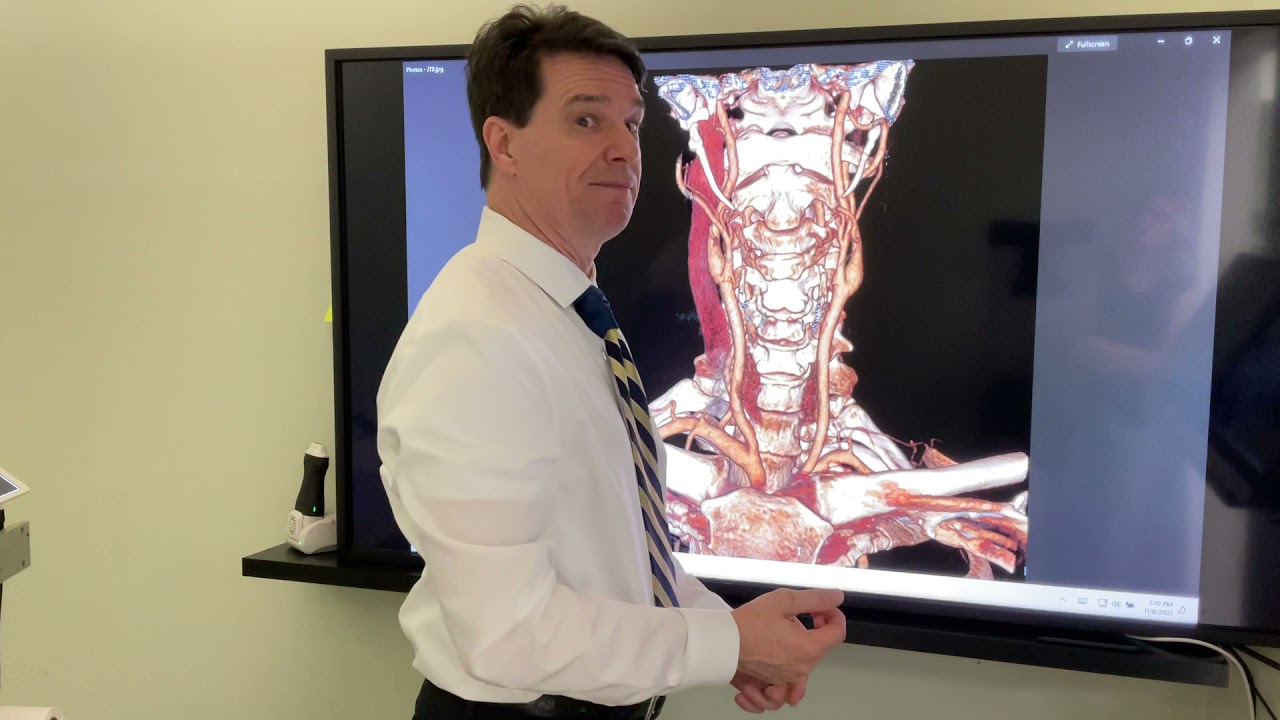
@jteleia By the way, do you know your video images is uploaded in YouTube. When I looked at, it looks similar to your images since I have looked into them a while back. See below link.
Hi @jteleia,
I’m sorry to read your struggles in France.
I’ve had surgeries with inexperienced/ignorant doctors here in Germany which I really regret.
So my my jugular compression was discovered very late and determined in the US.
In Germany or even Europe unfortunately very most doctors don’t recognize jugular compression as an illness.
In US they did a Doppler-Ultrasound to determine blood flow velocities between skull base and base of neck. Velocities > 50 cm/s where concerned to cause problems, about 25 cm/s are physiological as I read in literature. My velocities where about 100-110 cm/s. Because velocities and pressure are physically connected, you can assume pathological (venous) pressure inside the head, when velocities are that high.
In my case they had to remove styloids and also strangulating scar tissue that was wrapped around the jugular vein. If you could manage to see Dr. Hepworth in Denver that would be very best otherwise Dr. Heim in Bonn, Germany might be a good alternative, though he has no vascular surgeons involved. There might also be doctors in Italy treating jugular compression (by reading Research Articles). (Might be easier to get cost coverage staying inside Europe.) From my own experiences I can really advice against having surgery with less experienced doctors, especially then they don’t check for jugular compression with ultrasound or don’t want to shorten styloid at skull base. In my case that was all wasted time and effort.
Wishing you good luck finding help and symptoms relief. ![]()
Yes, I know he uploaded it and I have seen it posted here and have commented on it.
Thank you. I did talk with her about that and she definitely would take them back to the skull base. She’s saying it’s a 5 day hospital stay (in a place where I don’t speak the language) and is far from my home so I will have virtually no support so I am not excited about doing it twice (plus it will cost a lot more).
Thank you. That is so helpful. I had been in touch with Dr. Heim in Germany and several others in Italy and Spain and all wanted to operate right away based on my images and very little discussion. Except Dr. Heim who exchanged a few emails with me and assured me he was experienced with vascular ES. I didn’t pursue out of France care when I found out the procedure for getting it approved sounds pretty awful so I have spent another 6 months looking within France.
The ENT I am working with now says she not only is involving a vascular specialist but I specifically asked her if he would be in the surgery procedure and she said yes so that feels better. She is definitely planning to take it back to skull base and is willing to consult another ENT who does skull base surgery in the next month so she is taking my concerns seriously.
I just reviewed the flow measurements from the ultrasound the atlas orthogonal dr. did (the one in the video) and he said this:
“I believe the tech in France did a decent venogram for someone without your problem. You have such a significantly decreased flow in your left jugular vein that he needed to wait a little longer for the contrast to get through it.
Your left vertebral artery really opened up with the adjustment.
From 58 cm/s to 250 cm/s
and 44 cm/s to 186cm/s.
I did find some retrograde blood flow in the middle of your left jugular. A properly timed CT venogram will help to understand more.”
I did have another CT scan that was supposedly ‘held’ longer and it was pretty much the exact same result–no image of the left jugular but the recent ultrasound I just had done did find the left jugular was flowing, albeit less and even though it was more of a dynamic exam with different head positions, the angiologist said she didn’t see restrictions suddenly happening with different positions but she couldn’t tell if there was a compression. I haven’t gotten the results that would show the flow rates so I am very curious where you got your info about proper flow velocity b/c obviously from the dr. comments mine are way high right after an atlas adjustment (I was sitting up when he took it). Can you make anything of that?
What caused you to have strangulating scar tissue around the jugulars? That sounds scary. Sorry to hear your case was so difficult and resulted in multiple surgeries. Exactly what I am afraid of, not to mention long term damage to nerves and ending up worse instead of better.
That sounds like you found a doctor who is willing to help and is looking for the right things.
The velocities I mentioned are regarding to the internal jugular veins, that was maybe a bit misunderstanding. So it would be interesting what your velocities inside the jugular veins are. (You where talking about arteries where velocities are physiological much higher.)
In US they also did a cerebral angiography and cranial venogram with me for further investigations and because of a suspected narrowing inside my skull. Luckily the venogram showed only narrowings with pressure gradient between skullbase and c2 where the styloids were.
You are absolutely right with clarifying things before having surgery. I can’t recommend having several. So it might me good to get the venous velocities and maybe also have a angiography and venogram done. That is a bit more invasive and has it risks but might also give you and your surgeon a good reconnaissance. Additionally it might be good to talk with the surgeon about the US experiences with strangulating scar tissue that might have to be dissected from the jugular vein. As they told me there, the liberation of jugular vein on the outside is most important, much more then ballooning the vein.
Where the strangulating scar tissue comes from isn’t sure. That can have same reasons like styloid growth or calcification. In Colorado they have a special kind of tick’s fever that they’re suspecting as one cause for that scar tissue. Other lymphatic infections might be the next suspect. From my point of view the previous amateurish surgeries could be another reason or even the styloids itself by pinching the vein all the time. Unfortunately there is no satisfying answer yet.
Thank you for the clarification. I actually thought the dr. WAS measuring my jugular but I see now it was the artery–but I don’t know which one that is and how it might be affected by the styloid. He did measure something with the jugulars b/c he said the left one was flowing backward at one point (which seemed very strange/impossible to me). I sure hope the new ultrasound is measuring the velocities in the jugulars!
What do you mean the angiogram showed a pressure gradient? I’ve had 2 of them now and other than the images I posted, I don’t really have any specific pressure readings yet and now sure how that’s done.
I hope your scar tissue issue is much better now! Thanks!
It was a catheter angiography and venogram where they enter the vessels in the groin and go up all the way to the head. Then they are able to measure the pressure directly at point of interest.
Thank you - Last surgery was definitely a big relief for head pressure and connected symptoms.
Thanks. The AO dr suggested a manometry that sounds like the same thing but no one here seems to know what it is or the need for it. still waiting to see how much it would cost in the US or if I think it’s necessary.
Glad you have gotten some relief!