It was an evening in January 2016 when my wife & I came from a walk which was routine for us since she was 5 month pregnant with my 7 year son. As soon as we got home, I ran to the sofa and throw myself on it to sit. Within a few seconds, I felt what appears to be fluid movement at the back of my head and all of sudden, a feeling of extreme fear and doom hit me (can’t tell if it was panic or simple, partial seizure but never lost conscience during that episode). I ran to washroom as I was feeling confused and extremely frightened. I washed my face with cold water and ran to the fridge to grab a drink. after few minutes, the panic-like feeling subsided but I was never the same from that day on. The following 2 years, I was in what appears to be anxious state constantly and would easily break down. I was also smelling burning candles or coffee where there is none and also feeling of Deja Vu (this is a feature of simple partial seizure, not panic). I Could not concentrate on work and was preoccupied with finding out what really had happened to me. I lost a lot of weight in the process. I was also feeling tingling sensation in my back around T9-T10. I went to the doctor and explained what had happened to me, as usual my doctor prescribed buspirone (anxiety medication) as she thought it was all anxiety and panic that had hit me. The medication did a little to ease my constant state of anxiety and agitation. So I turned to meditation and life style changes which help a little but I was not feeling the old me anymore. Then in 2018, I begin to have insomnia, mild visual snow, floaters, halos/stardust around lights, ghosting, after images (palinopsia). I also started to experience loud tinnitus/pulsatile tinnitus and my sensorineural hearing loss, which was initially diagnosed in 2013 as mild to moderate, started to deteriorate to mild to severe. Right arm and right leg tightness and facial cheek muscles tugging/pulling begin to appear. Basically, all the IIH related symptoms showed up in full in 2018 onwards.
So now that I went through left Styloidectomy and C1 shaving without any noticeable improvement on my symptoms, I am beginning to think that , perhaps, the movement I felt at back of the head that day in 2016 might have been CSF leak and as result the brain might have slumped for a little while ( I am not sure about this but just my assumption). The reason is I did get an MRI imaging done for the hearing loss in 2014 (the oldest MRI I have) and it does show all the features of IIH along with what appears to be CSF leak in the facial canal which is linked to hearing loss (see the images below) but I was not feeling them at the time (2014). So while it is clear from the 2014 MRI, that I had IIH prior to the onset of my new severe symptoms, I am thinking what happened in 2016 might have been CSF leak presumably at the back of the head when I abruptly sat on the sofa. I could also be wrong and that it might have been totally something else like simple, one-time partial seizure (which BTW was ruled out when I did EEG in 2018).
So now I am at loss here. Trying to figure out what could this be. There is no doubt that I had bilateral IJVs compression and IIH (confirmed by imaging done thus far). I also have perineural cysts/Tarlov cysts in my cervical and thoracic spine which is linked to IIH and CSF leaks. So could I be suffering from CSF leak although I do not have orthostatic headache. My headache is more like pressure headache at the temples and facial tugging/pulling sensations towards the end of the day. My journey continues but I am beginning to doubt that this is all IIH related.
2014 MRI: Distended Optic Nerve Sheath (red arrows) and tortious optic nerve.
2014 MRI - Partial Empty Sella (Red arrow).
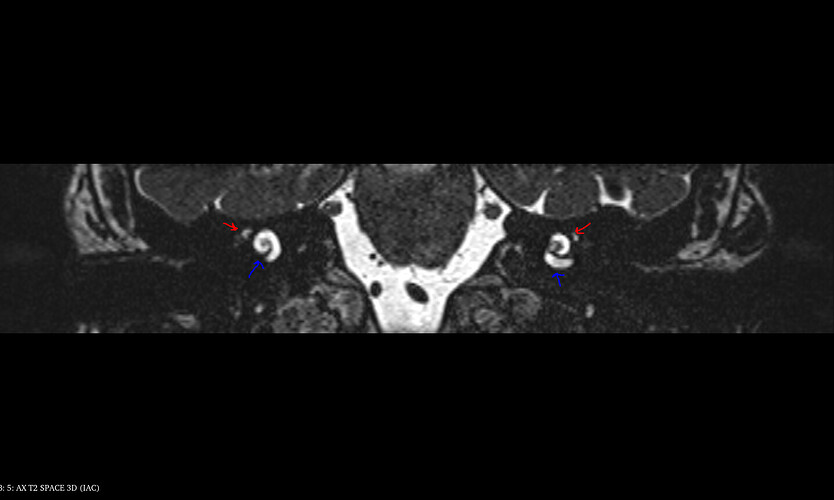
2014 MRI: Shows CSF filled dilation of the right & left geniculate ganglion (this is the canal that the facial nerve goes through) and it indicates meningocele (Red Arrow). This is linked to hearing loss and is basically CSF leak within the facial canal just above the cochlear (blue arrows).
Here is an image from the internet showing similar CSF filled geniculate ganglion of 64 year with bilateral sensorineural hearing loss just like me.
Source : https://www.ajnr.org/content/40/8/1402
Here is another study showing a 45 year old with bilateral sensory-neural hearing loss with CSF filled geniculate ganglion
Enlarged geniculate ganglion fossa in idiopathic intracranial hypertension
CLINICAL HISTORY
A 45-year-old female patient presented to the ENT department with a history of bilateral sensory-neural hearing loss, worse in the right ear. She was otherwise fit and well with no other reported symptoms. She previously had a CT examination following a head injury which was reported as normal at the time.
Source : Eurorad.org