Hi @Chan , I did take a look at the MRI video and compared it with the CTV video. First, I am not a doctor and although it is hard to conclude from 2 videos as to what is really going, my findings are based on what I see in these 2 videos.
Findings :
-
Based on these 2 videos, my conclusion is what you see as occlusion is an artifact of the T1 MRI. In T1 MRI, arteries and veins are indistinguishable from signal perspective since it shows the same signal for both of them. This is because, it relies on the volume of blood that is following in them which is about the same. So in this case, the occipital artery moves on top of the compressed but patent right IJV and their signals merge appearing as one and giving the impression that the right IjV has disappeared. The CTV, on the other hand, contains more slices and shows the compression of the IJV by the Styloid to be severe. It does not show any occlusion of the right IJV. CTV is done on venous phase, as result, veins appear more prominent than arteries. It also relies both the contrast and the volume of the blood that is flowing in the veins hence can accurately depict any occlusion as flow void. See the screenshots below for details.
-
I found what appears to be moderate sized arachnoid granulation in your right transverse sinus. I suggest you keep an on it so if it gets larger, it can potentially occlude the TS.
-
I found what appears to be the markers for IIH (raised ICP). I found Optic Nerve Sheath Dilation (ONSD) and Meckel Cave dilation. They can be better viewed in T2 MRI sequences as the CSF fluid is bright as opposed to dark in T1. These are both established markers for IIH as well as partial empty Sella which I think you found your self.
Hope these adds to your list of evidence to show that you indeed have the tale-tale signs of IIH, possibly induced by IJV compressions.
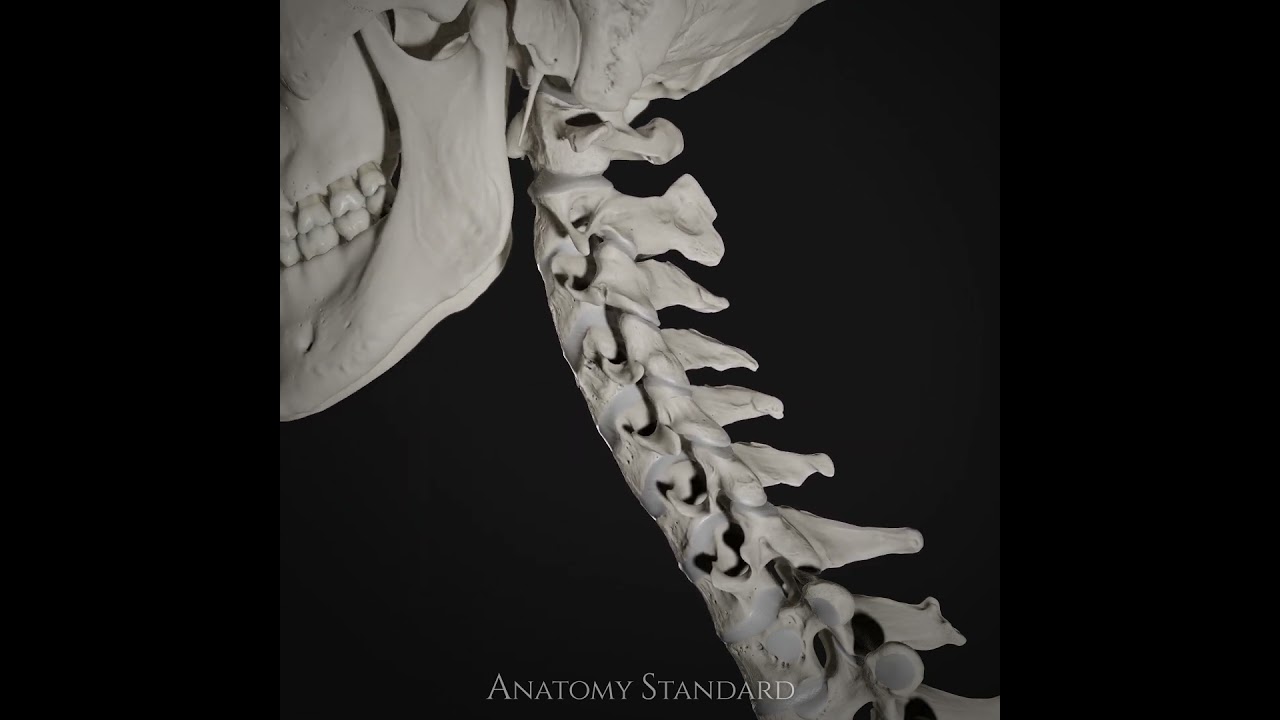
Here i see that the IJVs (green arrows) and right one is severely compressed by the Styloid(yellow arrows) mainly and to a lesser degree the C1(blue arrows - though small space appears b/w them) and you can see the occipital artery (red arrow) moving towards the right IJV. Reason I want to show the occipital artery is because it will move on top of the right IJV in the next images merging their signal and would be virtually indistinguishable
Here is the occipital artery (red arrow) just before it moves on top of the right IJV (green arrow). You can see the IJV is patent (open).

Here the occipital artery (red arrow) is on top of ( superimposed) the right IJV. The right IJV might be there its signal merged with the artery signal. That is an MRI artifact since the arteries and veins are isointense (same intensity or signal) in T1 MRI. Because they contain roughly similar amount of blood, it would be very hard distinguish based on their signal in T1 MRI.
Here is the CTV version
Here is CTV showing the worst compression of the right IJV(green arrow) by mainly Styloid (yellow arrow) and by the C1(blue arrow) to a mild degree. You can also see the faint signal of the occipital artery (red arrow). It is this artery that is more visible in the MRI when it moves across the IJV they have the same signal intensity, they will be indistinguishable. The CTV is done on venous phase, so the arteries won’t be prominent as the veins unlike the MRI where arteries and veins are Isointense (same signal) so when one transposes onto other, you will only see that. I would argue that the CTV is more accurate since it has more slices (299 slices) compared to the MRI. So since the CTV shows severe compression but not occlusion I do not believe it exists and it is mere MRI artifact.
Here I see Optic Nerve Sheath Dilation (Yellow arrows). Since this is T1, the CSF fluid is dark and you can see the dark lines (CSF fluid) that runs along with the optic nerve. This is sign of raised Inter-cranial Hypertension. It is best seen on T2 MRI as it will show the CSF fluid (the dark lines ) as bright white.
Here I see a moderate size arachnoid granulation (yellow arrow) on the right transverse sinus of questionable significance. You might need to monitor if it grows bigger, it does pose a risky of contributing to increased pressure in the brain.
Here is another II marker called enlarged Meckel Cave (yellow arrows). Since this is T1 MRI, CSF fluid will be dark and you can see that they are both enlarged but more pronounced on the right side perhaps coinciding with severity of the compression on that side. Indentation and Transverse Diameter (crossectional diameter) of the Meckel Cave: are considered imaging markers to diagnose Idiopathic Intracranial Hypertension as found on multiple studies.
Source Study : Indentation and Transverse Diameter of the Meckel Cave: Imaging Markers to Diagnose Idiopathic Intracranial Hypertension | American Journal of Neuroradiology