From @suenami21 -
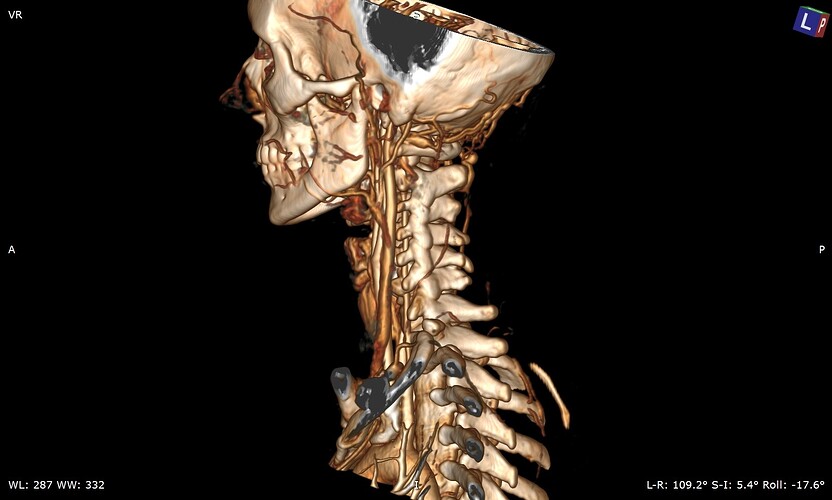
So my daughter had her icp monitoring done two days ago. They kept her at Hopkins until this evening and the results have not been officially given although they said that the fluctuations in her head pressure were not enough to consider it a problem with her csf so that is a good thing. Her pressure did rise significantly whenever she bent over or when her head went below her heart. Now we are left with the real possibility that the pressure has been coming from her jugular vein compression all along. We have a telecall with Dr. Costantino in early March so hopefully he will be able to look at her imaging and confirm that she does have compression at the C1 level. I’m not sure that her styloids are part of the equation but I think it is clear from the imaging that the C1 is involved. I’m going to upload many of her images that I was able to make into 3d with RadiAnt but I’m not sure how good they are. I would appreciate anyone who can view them to give me their opinion on anything they may see that could be causing her head pressure. I did include some 2D images as well because they do seem to show the C1 compression of the jugular.
Welcome, @suenami21!
I’ve annotated a couple of the images you posted & will explain what I see under each image.
On the left side, your daughter’s IJV looks compressed at the styloid/skullbase level, possibly at C1 then lower between C4-C6. Because her cervical spine is so straight, it almost appears the transverse processes of those 3 vertebrae are in contact with her IJV & even below them. She has quite a number of collateral veins in the area of her skull base which is an indication of IJV compression. Though I can’t see the very tip of the greater horn of her hyoid bone on this side, it almost looks like it could be in contact with her external carotid artery (ECA) which can cause different symptoms than the IJVs.
There are very similar situations with the right side though I can’t see enough of the hyoid bone on this side to comment about the right greater horn.
Her compression doesn’t look severe, but since she’s symptomatic, the compression is enough for her body to be reacting to it. That Hopkins confirmed its not high enough to be a problem is good & bad. Good because she’s at lower risk for a CSF leak, but bad because I feel, in some respect, they were saying IH isn’t causing her symptoms which it most likely is.
Dr. Costantino does IJV decompressions that aren’t associated with styloid elongation so it’s good that you have an upcoming appointment with him for your daughter.
@Isaiah_40_31 has been thorough as usual with her explanation & labelling, I agree that there’s compression at the C1 level & also lower down, so I would ask Dr Costantino about both those areas when you see him; it could be a blood vessel or soft tissue otherwise further down in your daughter’s neck…
Good you have an appointment and scans to show Dr C, I hope he can help her!
Thank you so much for looking at these scans and for pointing out the possible issues and labeling them so well. The details really help. I can say that her vascular surgeon, Dr. Khanjan Nagarsheth at the University of Maryland Medical Center has scheduled her for a jugular vein decompression surgery in mid March. He did a venogram of her jugulars and found that both sides are 97% compressed around the C5-C6 level. She had a fusion in this area in 2021 and he believes the veins are being compressed by scar tissue probably from that surgery. He said he thought there was going to be compression around the C1 area as well due to the cta images but he didn’t find this to be true during the venogram. I am not convinced that there is no compression there so we decided to continue to find other docs who focus on any neck compression issues that could be present. Isaiah_40_31 I also am concerned about the neuro docs at Hopkins saying her mmhg pressures were of no concern because of some of the high numbers that were recorded when she was bending over especially. They were well above what is normal for people who are exercising but they were only concerned about certain aspects of the recordings. They did acknowledge that they believe her when she describes her head pressure etc but they were only checking for potential csf leaks if I’m understanding them correctly. We’re glad that is off the table but it bothers me that they don’t know what is causing it and so far have not figured out what the next step should be to figure it out. I am convinced it is compression in her neck and skull base. Some of the drs have said they think that that could be the case but dont want to say anything definite. Dr. Nagarsheth is doing one side and then the other 6 months apart and may possibly need to put a stent in her vein. We would like to avoid that since he said he would be putting her on a strong blood thinner and she would not be able to come off of it for a year. So we are hoping that Dr. Costantino will see compression issues that he wants to address and we may have to postpone her surgery with Dr. Nagarsheth if Costantino can do all of what may need to be done. Add her wedding to the end of April and there’s alot going on right now. Dr. Nagarsheth said she has alot of large collateral veins which tells him this has been going on for quite awhile. Isaiah_40_31 I find it interesting that you are spot on with the collaterals as well as the compression between the C4-C6 area. That must be what he found in the venogram. Do her styloids appear to be wider than what I normally see on diagrams? They don’t appear to be very long but maybe the width is a problem in her case
That sounds like a good possibility. I reread an older post today where it was mentioned that for patients who tend to develop a lot of scar tissue, Dr. Aghayev in Turkey puts a layer of fat around the IJVs after decompressing them to help protect them from future compression by scar tissue. Dr. Hepworth uses sheep tissue to accomplish the same purpose. That’s to say that there are things that can be done during surgery to help protect the IJVs from re-compressing post op.
Based on my experience of 11 years on this forum, if a person is suffering from the symptoms we know go along w/ IJV compression, then I feel like diagnosis based on manometry readings from a venogram alone are not an adequate judge. I’m also not convinced that simply checking mmHg pressures in the IJVs can determine whether there are CSF leaks or not. It doesn’t necessarily need to be astronomically high to cause a CSF leak as there is variability in tissue thickness & strength in the brain in each person. There are sometimes obvious external symptoms such as clear fluid that drains from the nose or down the back of the throat or from the ear(s) intermittently. This fluid tastes salty & metallic. Does your daughter experience anything like that?
I agree with your conviction. It sounds like the doctors at Hopkins don’t know as much about the relationship between IH & vascular outflow obstruction as they should.
I understand why your daughter may need a stent, but I also hope she won’t need one.
I think it’s an excellent idea that you’re getting a second opinion.
Her styloids are very wide at the skull base & are not very well defined. I think that’s why her IJVs looked compressed to me right at the styloid/skull base junction, but you’ll need to see what Dr. Costantino thinks.
I agree that her styloids do look pretty chunky at the skull base, so it’s worth seeing what Dr C says, but be prepared for the compression further down to still be an issue? Stenting should be a last resort I felt personally, I’ve been very lucky that my IJVs opened up enough after surgery to resolve the head pressure…