Hi, my name is Sunil, and I am a 27 year-old male. I believe I have been experiencing Eagle Syndrome symptoms since around the end of 2014 but was never able to get a proper diagnosis. It got better and then got worse again. I’ve generally been in chronic pain for many years, but it got worse over time. I was more functional back in the earlier years even though I was experiencing pain, but since the beginning of January 2025, it started to get significantly worse day by day.
My history of surgeries includes: All 4 wisdom teeth extraction surgery done around the beginning of 2014.
Septoplasty for deviated septum done in Summer 2015.
Left lung wedge resection surgery done for spontaneous pneumothorax in August 2017.
Below is my story and symptoms from year to year. Sorry for the long post, I just feel like I should post my entire history to get advice and help from other fellow members.
Symptoms in 2014 include: Neck and arm pain bilaterally. At times, numbness and tingling that felt like brachial plexus issues. I had a cervical spine x-ray done, which came back normal. Sometimes, headaches or pain in the back of my head and eye pain. I would grind my teeth a lot during my sleep and eventually wore a night guard, so I also had jaw pain. I was also using the computer a lot every day and didn’t have the best posture while using it. I started working out with small weights during Summer 2014 and wasn’t stretching enough so I believe some of the pain may have come from that because that’s when I felt most of my pain start to trigger.
2015-2016 was a lot better pain wise, a lot of resting helped. I started to do calisthenics workouts (body weight training) in spring/summer 2016 and I felt good while doing the exercises but after a few months I felt like I slowly injured myself in a way because my neck and arms nerve pain started to flare up. On top of that, one of the pullups exercises I was doing triggered a spontaneous pneumothorax but ended up healing after a few days. After that incident I stopped calisthenics and became a little more sedentary. Also, teeth grinding stopped around this point in 2016.
2017 Symptoms: I started a college course that involved computers, so being sedentary was a lot more common during this period. But I also had a cashier/stocking job at the time, so I guess it was a bit balanced in a way. But I still continued to feel pain in my neck, shoulder, arms, mid back, lower back and trapezius more at this time and felt like any type of movement I did was painful. My posture still wasn’t the greatest. forward head posture was a big thing, so I tried a couple massage therapy sessions/ chiropractic and a little bit of physio, which relieved for a bit but didn’t completely help. Around Summer 2017 is when I got another spontaneous pneumothorax from stretching while I was lying down and went to the hospital to get an x-ray done. Doctors said it was a small tear/opening in the lung that filled up with air, but it wasn’t too bad and would heal in a few days. Weirdest thing ever. It ended up healing again but a few days after it collapsed again and after I went back to the hospital and decided that the surgery should be done to prevent future collapses. After around 2 months of healing, I was still a bit sedentary but also started working the same job again after my healing.
Ending of 2017-2018: I felt more buildup of pressure in the back of my head, deep in my eyes, minor facial pain, neck and arm pain, weird swallowing sensations and constantly feeling the need to yawn. I requested an MRI of head and neck from my family doctor to see if there’s any big damage that has been done. Like usual, they both came back normal according to my doctor.
2019 Symptoms: Still continued to feel the same, not worse but not any better. Around the end of 2019 is when I looked more into better postural changes and habits. I started moving my body a little more than the other years, and I slowly felt a little better, but not completely.
2020 Symptoms: Around March 2020 is when I quit my job due to the COVID-19 pandemic and started looking into calisthenics again. Since I was at home most of the time, I really tried to exercise and keep myself going. But even when I did calisthenics, there would always be nerve pain in my neck, arms, chest and an uncomfortable, slightly painful sensation in my face and eyes. I still felt like “pushing through the pain” but I just ended up doing more damage. I would use a backpack with books and small weights to do pushups, but all of that stopped when the pain started to increase around 2021. I stopped calisthenics again and the pain subsided but was always just there.
2021-2025 Symptoms: I didn’t want to tell myself it was chronic pain even though it had been going on for so many years, but I finally just accepted that it is chronic. My Ego got the best of me in some ways when it came to working out but at the same time there was never a true explanation for the symptoms I have been feeling. I started a job as a housekeeper in 2023 and although it was a really active job, I finally quit June 2025 due to “pushing through the pain” again. Throughout this period, I was also sitting and playing video games a lot.
2025 Symptoms: On neck rotation both sides, I feel eye and facial pain, like it’s impinging a nerve. Extension, flexion (If my head goes forward, especially if I start falling asleep while sitting, it feels like my head is slipping off my spine and I get this shocking feeling down my head and neck, that makes me wake up abruptly; lateral flexion pain increases. Chest, arm, neck, and shoulder pain bilaterally. Intense eye pain both eyes hurt when moving it in different directions/pain when blinking at times, facial pain increased. Some areas in neck/face, chest getting number day by day because the pain is so constant throughout the day, I feel like my nerves don’t ever get a chance to recover or rest. There is pain deep in my nose at times . My brachial plexus on both sides feels like they’re always squeezing. My brainstem feels like it’s being compressed at times, and it feels like blood flow is being cut off, and my head feels heavy/wobbly or like it’s about to fall off. I have not been diagnosed with cervical instability, but it feels like this may be another problem on top of possible Eagle’s Syndrome. Occipital neuralgia and trigeminal neuralgia feel like it’s also happening, but there is no diagnosis on that either. Swallowing pain increased and I get spasming at times. Talking is hard at times throughout the day because I feel pain in the back of my head, throat, and eyes, like some type of nerve irritation that disables me from talking properly. But there’s some days where I can talk better than others. I get burning in my face, neck and front of my throat especially throughout the day but then it goes away and comes back. There is an odd sensation in the middle and back of throat. TMJ issues, opening my jaw hurts the back of head (by my atlas and axis) and eyes, but it is very on and off. I have tinnitus in my left ear, which recently started this year, 2025. Every time I move my mouth side to side, I feel muscles/nerves getting irritated. Sometimes my tongue feels zappy/tingly and I get pain in the two front teeth. I have trouble breathing at times. I also have major problems lying down generally or when I have to sleep. The back of my head feels so sensitive on the pillow, and I also feel immense pressure in my eyes, neck, face and trapezius, chest area (kind of like everything is being pushed back). My quality of life has been significantly lowered, I am not able to do a lot of things I used to do, especially socially interacting and going out; not because I don’t want to but because I’m in pain most of the time. It very much has impacted my mental health.
Tests I have done and doctors/specialists I have seen.
X-ray- Cervical Spine 2015, 2018, 2022, 2025:
Came back negative according to radiologist, but all x-rays show straightening/loss of curve of cervical spine. My C2 bone has been malrotated to the left for a long time and also slight cervical scoliosis and right shoulder higher than left. Just was not mentioned by radiologist.
Throughout the years I have seen many different therapists, but only temporary relief was the outcome. Chiropractic, Massage therapy, acupuncture, dry needling, osteopath, and some physio.
MRI Cervical Spine – March 2025:
I got a cervical spine MRI ordered by a hospital doctor because although I asked my family doctor for neck MRI a couple years after the 2018 one, he denied because he was still going based off the one in 2018. The cervical spine MRI 2025 showed that I have: T2-T3 mild bulging disk and C5-C6 mild stenosis.
Chiropractic Biophysics - April 2025
I booked an appointment to see a chiropractor that deals with a more functional and mechanical correction of spine. He used different machines and exercises that involved mainly extension of the neck, but the pain started to get worse over the couple sessions. When extension of my neck was done or held in a stagnant extended position, it felt like nerves and muscles were being aggravated and caused more pain; so I decided to stop the sessions.
CT Scan Head and Neck with Contrast – June 2025:
I got a CT scan of head and neck done at the ER, but they were trying to rule out vertebral artery dissection. The report also checked for left and right carotid artery stenosis, cervical spine fractures/odontoid process/occipital condyles and neck tissues, which all came back “unremarkable”. No mention of styloid process length was reported. This was done in a still position, no dynamic head movement.
I’ve seen 3 neurologists throughout the previous years. When I explained to them the neck and arm pain I’ve been having, they performed an EMG test on my right arm, which came back negative. Throughout the years I’ve tried to explain more and more of my symptoms, but it was always just an EMG on my right arm and nothing else. Each time it would come back negative. Recently, this year, 2025, I have seen 2 neurologists so far. The first neurologist performed an EMG with a nerve conduction study (NCS) on my right arm. The only thing different this time was the NCS, but those results also came back negative. The second neurologist I seen did a little more than the others. Performed an EMG on my right arm and leg, ordered a Head MRI to look for multiple sclerosis, which all came back negative. Genetic testing was ordered, which I am still waiting for.
I have done blood tests to look for autoimmune or thyroid disorders, but it came back negative.
Dentist – Beginning of July 2025
I had a panoramic X-ray done, but the dentist did not mention any elongated styloid process, only some cavities that I got taken care of with dental fillings.
Upper Cervical Orthogonal Chiropractor – Mid July 2025
I made an appointment to see this chiropractor because he was the only one doing a Digital Motion X-ray (DMX) in the GTA. According to what was seen in the DMX, he said I don’t have cervical instability, but I may possibly have Anterior Atlanto-Occipital Dislocation. He recommended that I have a specific MRI done, but I am still trying to get a requisition from a doctor for it. This chiropractor was also looking for Eagles Syndrome but told me I didn’t have it. That is until I met with a NUCCA chiropractor in September.
Upper Cervical NUCCA Chiropractor - September 2025
I made an appointment to see a NUCCA Chiropractor and from the more specific x-rays he took, he told me I have Eagles Syndrome based on the length. He also said my Atlas is misaligned, so his goal was to get it back in place. I went to a couple sessions, but it still hasn’t helped.
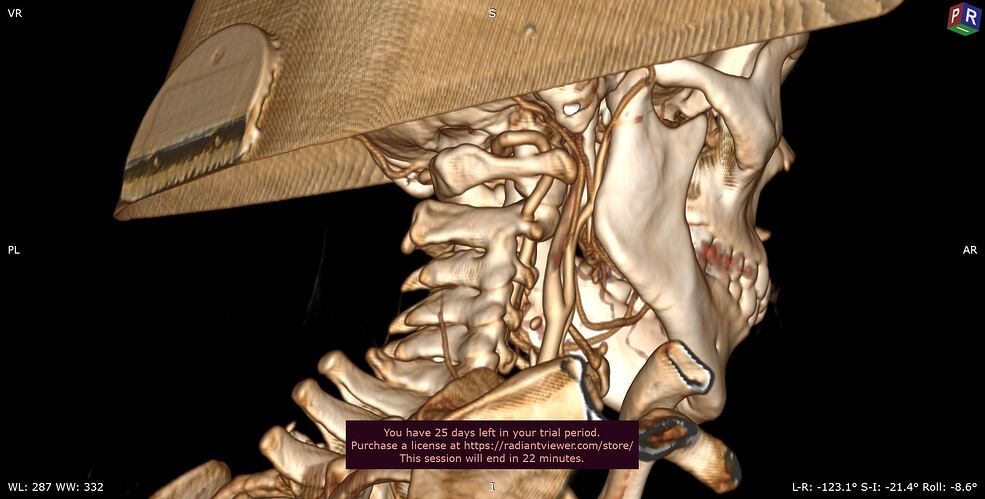
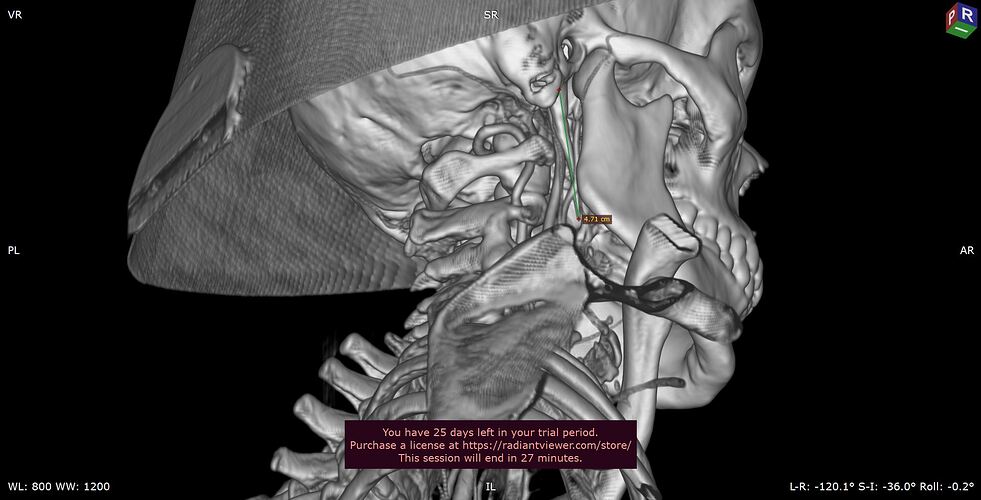
That’s when I started looking more into Eagles Syndrome and downloaded a program called RadiANT to 3D reconstruct my CT Head scan.
Medications:
Some medications I’ve tried were not consistent but used for some days. I’ve tried amitriptyline, gabapentin, pregablin, cyclobenzaprine (flexiril), duloxetine (Cymbalta) made me throw up so I discontinued it, diazepam, zopiclone (to help with sleep).
It really feels like the styloid processes are impinging my cranial nerves, and maybe my internal jugular vein (IJV) and internal carotid artery (ICA) at times. Below are some images of my scans. According to the scans, which other ones do you all recommend getting, concerning cranial nerve impingement, IJV and ICA compression and stylohyoid ligament calcification.
Panoramic Dental X-ray
NUCCA Chiropractor X-ray that identified styloid processes length.
Lateral Cervical Spine
3D reconstruction of my head CT scans using RadiANT
On my left styloid process, it seems to have a gap/separation. 5.07cm
Right Styloid Process (4.71cm)
Atlas Bone/Cervical Spine