@Buzz Thanks for isolating C1. It shows how well Dr. Lo carved a little groove without going too far into the bone. Also gives anyone thinking about this surgery an idea of what to expect before and after.
I appreciate your continued support. I know you keep saying it takes time and its up and down for the first few months.
As a side note to this, a friend of mine at work had a C1-C2 disc replacement for a bulging disc pushing on nerves. So kind of similar operation area. He thought there was something horribly wrong for the first 2 months and had a severe nerve impingement that made his foot numb. Slowly at about month 3 when the inflammation went down, he started to get the feeling back and had up and down days. He told me today at 6 months out he has made a massive comeback and feels great and there is no more tingling or nerve damage. He just keeps telling me give it time like you Isaiah ![]()
Thank you for your endorsement, @GCD! I’m really glad your friend was able to reinforce that “recovery takes time”.
Recovery from ES surgery is a true test of patience & requires effort not to be alarmed when symptoms go but come back (they almost always go away eventually). Some new symptoms can even crop up as the nerves heal. I sure remember this from my recovery!
After my endo/hernia surgery, it took me about 8 months to really feel like I was fully back on my feet and feeling the positive effects. I feel like surgeons can tell you about short- and long-term recovery, but the middle bit they always underestimate—it’s just not something they’re really involved in. I always feel like PTs have the most accurate assessment in those periods.
Hi all,
First off I want to say a big big thank you for all of the inputs here. I have seen over 100 doctors in the last 10 years, 2 failed neurosurgeries (Chiari and C1-2 fusion) and loads of opinions! At this point I have seen Dr. Athos Patsilades (once in 2021 where he did a venogram and suggested I see his colleagues in neurosurgery), Dr. Nicholas Higgins (who also suggested c1 shave only) and Dr. Amir Dehdasthi + Constantino (who I am seeing again next week. Given my history (7+ years of misdiagnosis) and still recovering form the C1-2 fusion (which has a whole set of complications of it’s own, some life altering), I’m hoping to get some input/support from the group here. My symptoms are severe, including unbearable memory loss/brain fog, fainting episodes, visual obscurations, and pulsatile tinnitus. To top it off, my family has dismissed me as hypochondriac, despite the fact I’ve been approved for multiple venograms and have abnormal imaging.
@KoolDude @Buzz , if you are able and have the time, or any other member, would you be able to take a look at my venograms and CTVs? I have had a variety of opinions, some of them (Dr. Lo) saying my right side was open enough to compensate. Others (Dr.Hui, Higgins, Dehdashti) saying my compression is bilateral and that I would need surgery on both sides to address the C1+styloid. Dr. Higgins also said I have some compression of the left bracioencephalic vein (I’ve had crazy specific MRI’s to evaluate for TOS that have confirmed this as well). Am I not understanding the scans correctly? Is the compression minimal as Dr. Lo seems to think? Is one sided compression enough to cause symptoms? I tried to use Radiant software but it is not compatible with my MAC.
For those of you who have vascular eagles, have you seen Dr. Dehdashti+Constantino and how was your experience?
I’ve attached a link to all of my studies (CTA/ MRvenogram from 2021) in addition to some screenshots of an MRI of the neck/head.
Many thanks to any one who can chime in on my images! I know vascular eagles to be very complicated, and many surgeons are not touching the C1 due to it’s very precarious location on the body and proximity to important arteries.
@minabee Do you have any of these symptoms: dizziness, vertigo, imbalance, Hemiparesis ( weakness or the inability to move on one side of the body).
@minabee - Your link doesn’t work. Uploading your scans on dicomlibrary.com is a good way to share your images. Dicomlibrary anonymizes the images & will give you an individual link to share for each set of images you upload. A lot of the recent images you’ve seen on our forum are from dicomlibrary uploads. A scan w/ lots of images such as an MRI or CTA can take awhile to load so I recommend starting the upload at night so your computer can work all night. You’ll also need to set your computer so it doesn’t go to sleep. I have a Mac & uploaded images to dicomlibrary so I know it works w/ Macs.
web link work / i m look
Thank you @anon67578920. Please let me know if you think anything is of concern or if I have gone after the wrong diagnosis.
Hi @minabee, I have looked into most of your images for the past couple of days. You really had all the imaging one can possible have. I think I found something that I suspect might be responsible for some of your symptoms but I did ask you if you had additional symptoms other than the one you listed which I did not get an answer for yet. However, I think you are suffering from a compression of Medulla/Brainstem by your left Vertebral Artery (VA). Your left VA is thick and your right VA is hypoplastic. This compression of brainstem by the left VA can produce a lot of symptoms which includes dizziness, vertigo, imbalance, Hemiparesis ( weakness or the inability to move on one side of the body), syncope/passing out…to name a few. basically these symptoms stem from higher cord (spinal) compression symptoms (myelitis symptoms) and intermittent vertebral artery blood-flow disturbances (vertebral insufficiency symptoms) which produces the fainting symptoms (syncope) you described.
I do believe this could have been what is mimicking Eagle syndrome.
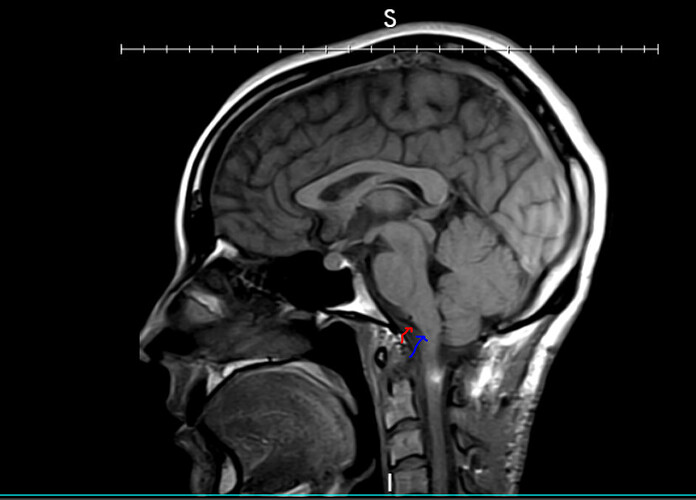
Here is axial, sagittal & coronal slices showing the left vertebral dolichoectatic (Dilated) artery (red arrow) compressing the Brainstem/medulla (blue arrow) and you can see the high intensity signal area (green arrow) indicating that the brainstem is under pressure of the compression by the left VA. The first axial T2 FSE slice is showing it clearly as you can see the shearing of the brainstem to right by the force of the artery.
*Here is your 3D rendering of one of your CT and you can see that your left VA (red arrows) is thicker and angled inward towards the brainstem which is responsible for the compression of the brainstem/medulla. You can also see the right hypoplastic VA (green arrow).
Here are your IJVs. I think I agree with Dr Lo, Your right IJV (blue arrow) is the dominant one and draining most of your brain and it is slightly indented by the C1 (red arrow) & Styloid (green arrow) but widely open (patent). Your left IJV (blue arrow) is smaller and is compressed by the styloid(green arrow) and C1 (red arrow). So I believe the right one is compensating very well since it is the one draining the most. I could not also see any IIH markers which makes me doubt you have IIH related issues.

I can also see the left brachiocephalic vein (green arrows) compression between left clavicle (red arrow) and left Common Carotid Artery (blue arrow) and right brachiocephalic artery (yellow arrow). But since left IJV is smaller one and it drains into left brachiocephalic vein, the compression of left brachiocephalic vein should not pose much of an issue. your right brachiocephalic vein compression would have been significant since your right IJV is the dominant one and drains your brain mainly.
Finally, you need to investigate your left vertebral compression on your brainstem. I believe this is the cause of most of your issues. It can also mimic number of diseases including eagle syndrome since the symptoms overlap.
Here is couple of internet article to read to see how you compare and educate yourself
Source of the Study : Vertebral Artery Compression Syndrome - PMC

Source of the Study :https://www.thieme-connect.com/products/ejournals/pdf/10.1055/s-0043-1769899.pdf
You are very knowledgeable and kind kooldude, to take the time and help. Quite amazing! Thank you for the information.
@GCD i hope you don’t mind hijacking your thread here to help another fellow.
@minabee here is a case of 36 year old who had fainting spells (syncope) as result of brainstem compression of right VA. You can see the images and read about it in the study link below to compare your case.
- Introduction
The clinical significance of neurovascular compression has been explained by Jannetta, who linked it with trigeminal neuralgia. According to his theory, both the compression of nerve V and pulsatile blood flow in arteries affected by atherosclerosis and age-related elongation cause irritation and hyperactivity of this nerve [1]. Currently, neurovascular conflict is a commonly known clinical condition associated with disorders such as trigeminal neuralgia, hemifacial spasm and glossopharyngeal neuralgia [2]. Vertebral artery medulla compression syndrome (VAMCS) is a condition of significantly lower prevalence and more severe clinical course. The complex clinical presentation of VAMCS, as well as the frequent asymptomatic modeling of the brainstem by the vertebral artery (VA) [3], requires meticulous diagnostics. It is necessary to prove that the symptoms result from the compression of the brainstem by the VA, and clinical conditions such as brain tumor, stroke and multiple sclerosis should be ruled out.
In this paper, we report on the case of a young patient with symptomatic VAMCS. We also present a review of the literature concerning VAMCS with special attention paid to clinical symptoms, diagnostics and therapeutic methods. Cases of brainstem compression by VA aneurysm and compression of the upper cervical spinal cord were excluded from the analysis.
- Case presentation
2.1. History and examination
A 36-year-old male with a history over the last six months of limping on his left leg and touch sensation impairment in the left half of the body presented with left hemiparesis. Over three months prior to admission, he experienced two episodes of syncope. During this period, the patient complained of paroxysmal ‘‘lightning’’ pain provoked by physical effort and neck flexion in the right occipital region extending to the opposite side of the body with concomitant nausea and periodic vomiting. Similar headaches appeared two years previously and spontaneously remitted after several months. On admission, neurological examination disclosed sensory loss to pain, temperature and non-discriminative touch on the left side of the body. Mild left hemiparesis with increased muscle tone and ankle clonus were observed.
2.2. Imaging studies
An MRI of the head revealed compression of the ventrolateral aspect of the medulla oblongata by an elongated and tortuous right VA (Fig. 1A–C). There were no pathological contrast enhancement or diffusion restriction regions in the brain. CT angiography and DSA (Fig. 1E) disclosed the loop of V4 segment of the right VA projecting posteriorly. Diffusion tensor imaging (DTI) demonstrated the compression and medial displacement of the right pyramidal tract at the level of the upper medulla oblongata (Fig. 1D). A post-processing tool (the syngo.MR Tractography, Siemens, Erlangen, Germany) was used for DTI analysis. ROI-based analysis was performed on the medulla oblongata to reconstruct the pyramidal tracts. Based on MRI, CT angiography and DSA, other conditions such as tumor, aneurysm and multiple sclerosis were excluded.
Source Study: https://core.ac.uk/download/pdf/268477133.pdf
Post deleted by Moderator due to personal information availability
This looks so cool! Was it made with Slicer3D/plugin or some other software?
Hi @vdm , good question I really do not know what software it was made with. It came in with one of minabee’s CTA’s(there were many CTA/CTVs). I think whoever did that CTA had software which rendered in 3D.
Initially I thought it was Vesalius 3D (based on marketing material it has super duper features, like “scissors” in 2D planes that reflect in 3D volume in real time, sort of advanced option of 3D “scissors” available in RadiANT viewer. But the metadata in the screenshots are displayed a bit differently than in the one above, so perhaps it’s something else. I couldn’t quickly find anything alike on Google, so it might be some proprietary tool.
Yeah, I think it is proprietary tool. If you think about it. It is not that complicated. All it does is superimpose the vascular system on generated skeleton so one know where the vessel is located relative to the skeleton in the background.
I think 3D slicer is much more complex and advanced since it comes in with many vascular plugins (extensions as they call in 3D slicer) which can do a whole lot. The only down side to it, it is not user friendly and the learning curve is steep.