Hey, I’ve been reading on this great platform for some time now, and today I want to share a bit about my symptoms, the imaging I’ve already undergone, and so on. I’m 22 years old and from Germany, and I’ve been experiencing various symptoms to some extent for probably over a decade. I attribute some of the symptoms to CCI, which I was recently diagnosed with, some to a cerebral outflow problem (internal jugular vein), and some I don’t really know the cause of.
Some of my symptoms:
• cognitive dysfunction (probably the most important symptom), they vary greatly over the days, weeks and months but are always present:
◦ Brain Fog
◦ intense restlessness
◦ Derealization, dream-like or trance-like states
◦ feeling like drunk
◦ poor executive functions
• permanent pressure feeling in the head, especially forehead area (worse with bending over)
• pulsatile tinnitus (both sides) which only occurs with exertion and rarely while lying in bed
There is definetly a strong connection between the pressure feeling and pulsatile tinnitus as on very rare days I don’t feel that head pressure and if that is the case, the pulsatile tinnitus also doesn’t occur with exertion
• headaches of different types and locations, sometimes only one side, especially right side
• neck pain
• loss of gag reflex and reduced sensation on the right side of my throat (especially noticeable with cold drinks)
• visual snow and eye floaters, sometimes the eye floaters greatly increase, especially in phases of strong derealization
• phases of overly sleepiness and on the other hand phases of insomnia
• face swelling
• muffled hearing
• Flushing of face, upper body, arms and fingers
• hard little lumps in fat tissue in upper arms, chest and abdomen
• ……
As I mentioned previously, I have already been diagnosed with craniocervical instability, which was challenging to diagnose in Germany. While the doctor believes that these symptoms are caused by CCI and the irritation of the autonomic nervous system, I’m skeptical that this is the entire explanation.
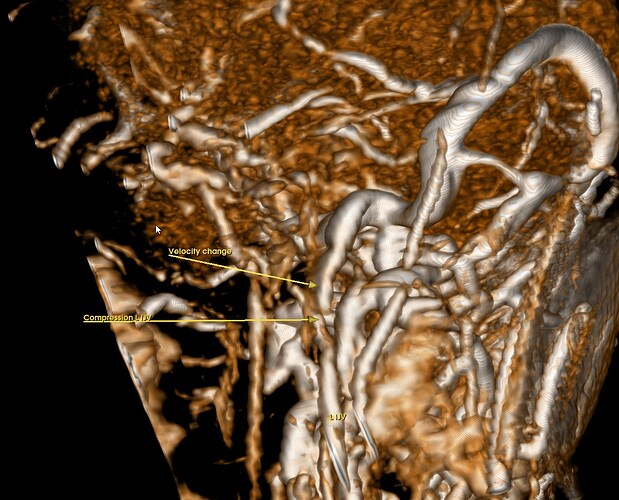
I also suspect some compression of the internal jugular veins, and I believe there are indications supporting this hypothesis in some of my MRI images. These MRI images include venography without contrast (2D Time-Of-Flight). According to the radiologist, there is nothing remarkable to note in these images. However, I would appreciate hearing your opinions on them, especially since many of you may have had similar experiences where significant findings were initially overlooked. As of now, nothing regarding a potential IJV stenosis has been confirmed, it remains speculative. An unusually long styloid process couldn’t be confirmed with an X-ray.
I have included images of the MRI (t2 sagittal, ToF 2D venography, and 3D Reconstruction of the 2D ToF), with arrows and labels indicating points of interest.
Left side:
On the left side, it’s noteworthy that the left internal jugular vein (IJV) can be seen below the compression (only visible in the 3D reconstruction image).
Right side:
The right IJV can’t be seen below the compression, probably the compression is more severe on this side
GIF of the 3D Reconstruction:
The collateral veins seem big compared to the internal jugular vein.
I hope to have a CTV/CTA very soon, and hopefully, the picture will become clearer by then. I will post them once I have them done.
I already know that I have a arcuate foramen (I don’t know if it is bilateral) and it could probabably explain the one-sided headaches I sometimes get but I don’t think it contributes to the other symptoms.
Also CSF leaks could be involved as I rarely get clear outflow out of the nose when bending over. I also sometimes have fluid sensations in the ear, but no outflow.
I also speculate if some autoimmune stuff or MCAS could be involved, especially because of the flushings (especially in stressfull situations) and other symptoms like feeling very hot and these little lumps in the fat tissue. This could potentially explain the instability of the cervical spine, shoulders, and other joints. Although I don’t experience significant joint pain, they sometimes feel unstable. It’s not the sensation of stretched ligaments but rather the tendons that seem to be affected, particularly noticeable in the jaw region. The jaw feels unstable, particularly next to the TMJ joint where the coronoid process sits and the tendons attach. There isn’t much information available on this yet, but concerning CCI, there are speculations about tendinous instability.
I also considered whether a genetic disorder like EDS could contribute to this hypermobility. However, unlike typical EDS presentations where fingers are often affected, mine aren’t. Interestingly, I’ve had five supernumerary teeth (not counting the wisdom teeth), which is occasionally documented in individuals with EDS.
I have noticed that cold showers help me immensly with many symptoms, especially the cognitive symptoms. Also caffeine paradoxically does calm me down. I contribute both to effects to the autonomic nervous system.
Thanks for reading and for being a part of this fantastic forum!