Hello!
I recently have been fortunate enough to have had consultations with Dr. Hepworth, Dr. Costantino, and Dr. Nakaji. It did take quite awhile and bit of effort to make it happen, but I am glad to have had the opportunity to meet with each of them.
Overall though, after meeting with each of them, I am feeling fairly confused and discouraged. The combined summary is basically Hepworth and Costantino feel strongly about moving forward with surgery and Dr. Nakaji declined surgery and thinks I should explore other options first. I’ll go in a little more detail if that’s okay and maybe y’all can help me out, offer encouragement, or just commiserate with me.
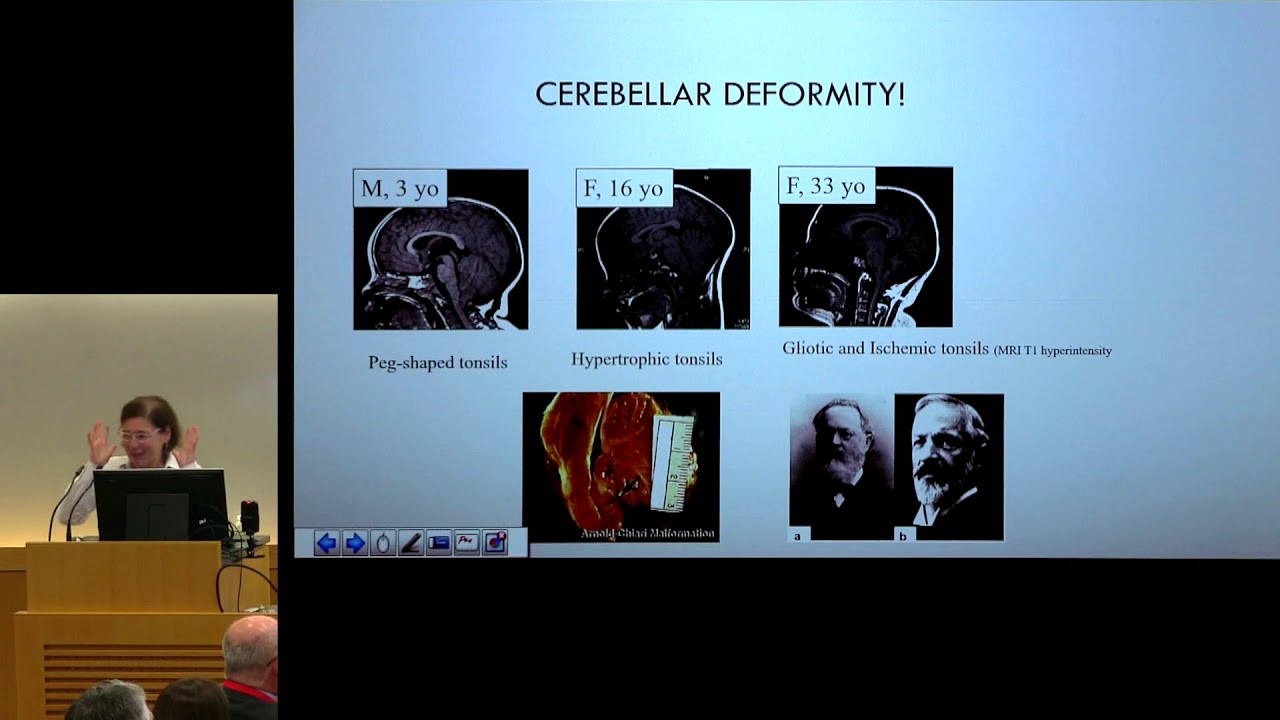
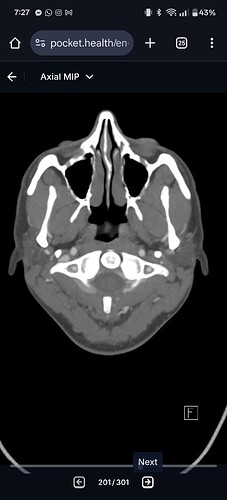
HEPWORTH: Visit with Dr. Hepworth included review of CTA and Doppler Ultrasound and he concluded that in regard to the CTA: left jugular vein is absent, right jugular vein is diminutive, right transverse sigmoid sinus with an arachnoid granulation. He also noted a strong possibility of tethered cord, and low-lying cerebellar tonsils.
In regard to the Jugular Ultrasound: Right: Base of Neck 150.3 cm/s ; SCM 187.6 cm/s ; Carotid Bulb 26.8 cm/s ; C1 31.5 cm/s ; Foramen 48.0 cm/s Left: Base of Neck 75.5 cm/s ; SCM 83.2 cm/s ; Carotid Bulb 0 cm/s ; C1 0 cm/s ; Foramen 0 cm/s
I’m not sure if any of those numbers make sense to any of you, but it sounds like the right flow velocity was elevated to some extent, and on the left they could not obtain measurements at certain points. He went ahead and got me on the surgery schedule later this year, so it seems like he feels pretty confident about the issue. His notes say, “Recommend a right styloidectomy with jugular vein decompression first…Discussed there is a chance of doing a left styloidectomy/venous decompression in the future.” He was the doctor who prescribed me Brilinta (blood thinner) which I feel has worked better than I originally thought (when I went off it, I noticed more brain fog, worse headaches, increased visual snow), so I asked to stay on it.
COSTANTINO: I really liked Dr. Costantino, I felt he was straightforward but also compassionate. He reviewed the CTA and Doppler Ultrasound and said that the right side was significantly compressed by the styloid process and the left vein was hypoplastic. I don’t have his notes, but he said my case was a “no brainer.” I had had the dynamic cerebral venogram done the day before, so I didn’t have Dr. Mehta’s notes yet, but I let Dr. Costantino know Dr. Mehta’s thoughts. He seemed hesitant about the results because I was under sedation and he would have preferred a balloon venogram (or something like that). He said that he wouldn’t have even ordered the cerebral venogram though (done by Dr. Mehta) because he felt like the imaging I had sent him, along with the symptoms I was describing, were already convincing enough. Dr. Costantino felt the Brilinta was a pretty risky drug to be on because it is a blood thinner and said I should really consider the benefits vs. the risk.
Dr. Nakaji/Mehta: I really pushed to have the cerebral venogram done and to have a consult with Dr. Nakaji because I want to make sure I’m making the wisest decision regarding treatment, and also Dr. Nakaji is familiar with another condition I had called Chiari Malformation. I thought he would be an ideal person to speak with.
The cerebral venogram/catheter venogram went fine and it wasn’t too uncomfortable. They gave me enough sedation that I could acknowledge them when they asked me to turn my head, but otherwise I was pretty much unaware of them fiddling around. Except, I think when they put in more contrast or something, I would feel these rushes or waves of burning in my head that did not feel good (enough to where I had scrunch my face ![]() and I usually don’t have to do that unless it’s a severe headache). I’m not sure if that is normal, but I figured it must be because it is a fairly extensive procedure.
and I usually don’t have to do that unless it’s a severe headache). I’m not sure if that is normal, but I figured it must be because it is a fairly extensive procedure.
Anyways! I felt sure that the results would be agreeable to Dr. H. and Dr. C.’s opinions. However, my results from Dr. Mehta are:
“Dynamic cerebral venogram performed with Dr. Mehta shows - the left jugular vein is thrombosed, with the right one open and only with minor stenosis and no significant gradient across the jugular vein including with provocative head positioning.
While there is stenosis of the right internal jugular vein which is dominant at C1-C2, there is no significant pressure gradient in neutral position. With head flexion there is a pressure gradient of 2mm Hg from C1- C4.”
Because of that, Dr. Nakaji’s consultation resulted in the opinion of: “We discussed that although there appears to be a focal point of compression on CTV, it is not severe and there is no pressure gradient on venogram. As such, it is unlikely that she would benefit from jugular venous decompression.” And then he recommended I look into other headache therapies (which unfortunately I have, but I listened to him because he is an expert and I take his opinion seriously). Dr. Nakaji also felt that there was probably no need for me to stay on Brilinta.
ULTIMATELY, all of the doctors seem to agree my left vein is not very functional, but have differing opinions on the right vein. But honestly, I’m not sure what to think if the pressure gradient aren’t high or indicating an issue? Regarding the left one being out, I know some people function on only one and that is not necessarily dangerous in itself and they are healthy and okay? I’m wondering if maybe I’m just one of those people who has a harder time than others for some reason, or maybe like Dr. Hepworth discussed, it could be a combination of issues working together. I’m not really sure. Or what is IJV compression isn’t my issue at all?
My plan is now to send of Dr. Costantino the results from Dr. Mehta’s testing and hear his thoughts. He wanted to meet again, so I’d like to go ahead and try to get that appointment scheduled. I already have an appointment scheduled with Dr. Hepworth in August.
Anyways, I left Dr. Nakaji’s consultation feeling appreciative but also discouraged. Wondering if anyone has any help or guidance, or encouragement. Thank you!