Hey folks, grateful to connect with you all. TLDR below.
I’ve been on a hellish journey and I know y’all can understand the feeling. Here’s a novel describing most of my issues prior to now:
I’ve had (mostly) right sided ear pain all of my life, tubes as a kid, and developed tinnitus in my teens. 16 years ago I saw OMFS for charlie horses under my right jaw and pain in my right face in general– received the ubiquitous TMJD and myofascial pain syndrome dx and was instructed to use my fist to keep my yawn smaller, which mostly works for the spasms, yay. In my early 20s I checked in with ENT about constant right ear pain, and docs told me “eustacian tube dysfunction”–cool, I’ve got allergies, that makes sense. Fast forward a few years and it turns out I had a golf ball sized benign tumor removed from my right maxilla – fwhew, that must’ve been it the whole time, thanks doc.
Annoyingly, as I’m sure you’ve all experienced, in general, the symptoms persisted and worsened. Right eye pain starts coming on, then the visual distortions set in (pulsing vision, trouble holding gaze on details), and many many workups reveal nothing much to speak about… “You’ve got dry eye, use these eye drops”. I learn about “visual snow syndrome” which explains the dots I thought were atoms as a kid. Then began the sense my right lung wouldn’t inflate fully at the base somehow, like my diaphragm wasn’t working right–as a musician of many years I was intimately familiar with how it felt to use my diaphragm, but another extensive work up didn’t show much past bad asthma. Along with mostly right sided headaches?–I’ve never been sure what to call them–but my head often feels heavy and I have one kind of pain in the back of my head/upper neck, and a fairly common throbbing in my right eye/cheek/upper clavicle/ear area much of the time, usually much worse when laying down. My PCP ordered many tests which came back largely unremarkable. Clearly I must be bonkers, health anxiety isnt uncommon, so I spent a lot of time and effort convincing myself I merely have anxiety and to chill…. maybe meditation will make all these painful sensations go away.
A few years later I am diagnosed with a rare genetic connective tissue disorder, which seemed like it could be the issue. While some symptoms weren’t explained, for instance when bending over my right face starts throbbing and my right eye feels like it’s being punched from behind. My visual issues seemed worse, as though the world pulsed with each heart beat. The doctors said avoid bending over so you don’t have the sensation. Okay…
Fast forward to 2 years ago and I start feeling like I can’t quite swallow properly… on the right side. The other symptoms remained, but I’d come to accept I’m a lunatic instead of sensing something outside of my brain. Food felt as though it was getting stuck, and I knew I had felt a slight choking sensation when turning my head toward the right but by this point it was a very strong choking sensation and came with a variety of stabbing/pulling/object sensations… in my right neck, but also radiating to my lower tongue, gums, ear with sensations of fullness and tickling and tingling, up my cheeks/cheek bones/temples, even stretching down to my shoulder a bit. This is undeniable–never have I had to take multiple swallows for food, and my ear had never felt like I was sitting on my foot. Infection, maybe, since I’m clearly crazy and they’ve scanned everything??? So I go digging around in my tonsils with a q-tip to check for tonsil stones and see a white cyst on the tonsil… aha, that must be aggravating my throat. I see 2 private practice ENTs who can’t find the cyst and suggest I see a therapist, and a third at an academic institution who says “Oh yea there’s the cyst right there… but I think it’s a red herring. This sounds like eagle syndrome or glossopharyngeal neuralgia, let’s get a scan, and I’ll send you to my colleague who knows a bit more about ES than me”.
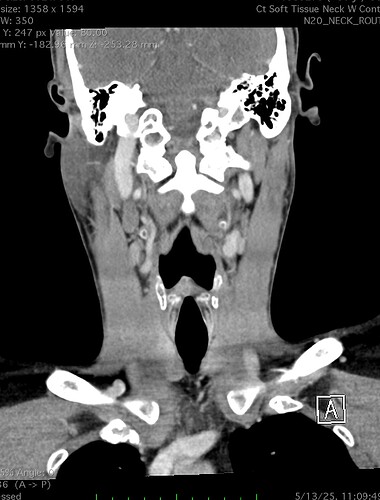
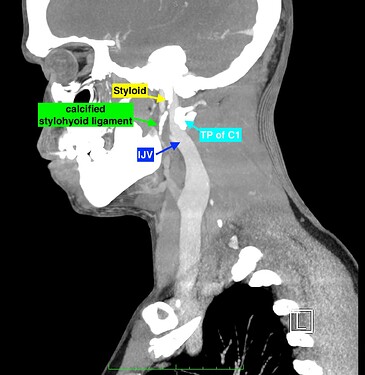
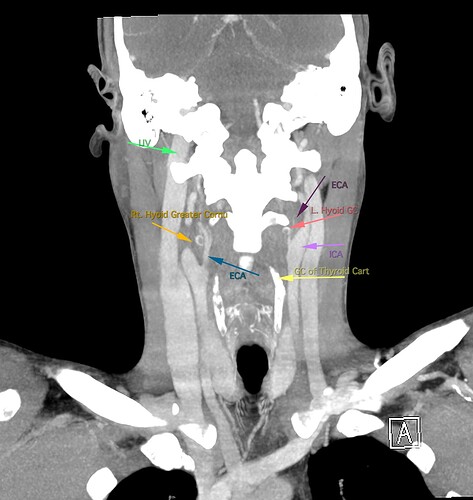
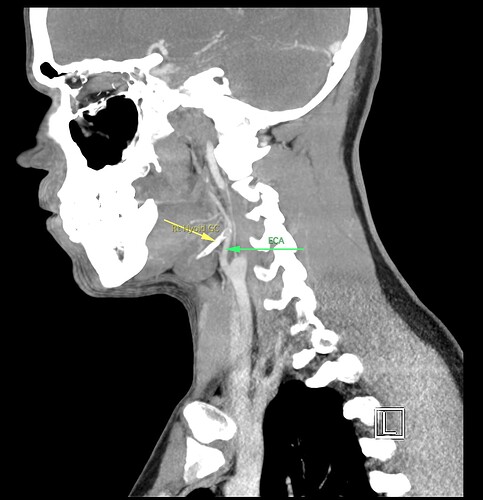
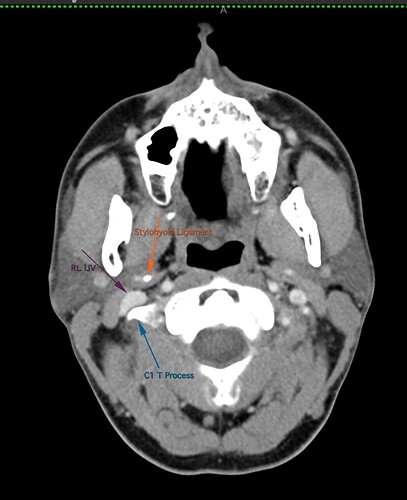
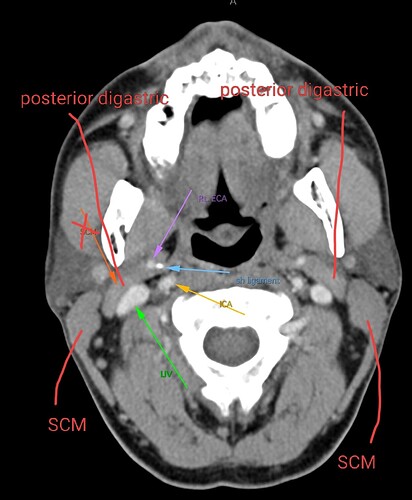
So, 2 years ago was the first time I came across Living with Eagle, filled with descriptions of all my symptoms, and a slew of scans showing very obvious bone chunks in the neck. Since I studied bio in college, and these bones are obvious, I figured I’d take a stab at looking at my own past scans and, low and behold, mild–but present–ossification of my stylohyoid ligament. Perhaps more relevant in my case, in the process of learning enough of the anatomy to understand axial images I noticed another weird thing–my right external carotid artery is in the wrong place. Instead of sitting lateral to my hyoid greater cornu, it’s medial. Hmm.
Now, of course, neither of these pieces of information were included in any radiologists report, so I bring it up to the slightly-more-familiar-with-ES ENT and he goes “eh, I’m not sure Eagle Syndrome is real, and it sounds like the surgeries for it often don’t resolve symptoms, so lets just take out your tonsils”. Okay, reasonable, he’s the boss, I’ve had tonsil stones, I’ll do anything to resolve the pain. By then, I was also getting flashes of white light in the corner of my vision and ever-more-regular pulsations in my right face/head/neck, so pretty much would do anything to feel like my brain wasn’t rotting in my head.
Tonsil surgery did solve the problem of my tonsils hurting, because they were gone, but no resolution of other symptoms. This was a year ago. I’ve been to PT, SLP, and now back to PT while I trial gabapentin for the neurologist. PT#2 discovered a bunch of significant atrophy in my upper right shoulder/back, and, you guessed it it’s all right sided. I’ve since then, thanks to radiopedia and Netter’s, also explored my images and noticed a few other anomalies in my scans, including an extended right thyroid superior cornu which appears to be pressing strongly into my neck also in the general area of pain, and an occipital artery branching off and wrapping around the internal carotid. Frustratingly these also weren’t mentioned on rads reports. My swallow study by the SLP showed obvious asymmetry with my swallow, but the SLP reported it symmetric and radiology apparently doesnt read the A/P view in their modified barium swallow studies? This is not inspiring faith in the academic institution I attended, but what can I possibly know they dont?
I’m here cause I’ve learned so much, and ya’ll seem to be the internet experts of weird head/neck issues adjacent to the stylohyoid chain. The docs keep seeing me, and keep ordering imaging, and seem to not be talking to each other at all? Frankly it seems to me the answers are in already in the images… so I’ve included several, perhaps you’ll see something helpful and can offer a suggestion… I just know I’m exhausted, frustrated, in so much pain all the time I cannot function which is so demoralizing, and it’s getting worse despite physician recommendations.
There are lots of random other symptoms: my right jaw feels like it’s hanging at the joint, and I catch myself resting my tongue between my teeth to stabilize. I have constant pulsations in clavicle shoulder area, right, especially when laying on right side… many symptoms seem worse, like eye dancing, head pulsations, etc. I can’t sleep through the night anymore due to neck discomfort waking me up. Any light pressure on the right side of my neck feels like choking. I often feel vertigo, like my right eye wants to roll back in my head and I’m being pulled backwards. Tinnitus is non stop, and when I eat/swallow/wear headphones I get pulsatile tinnitus. Pain on swallowing is near ubiquitious. I’ve started getting these brief episodes of ear fullness with heavy ringing and going mostly deaf to outside noises, which last 10-20 seconds. When turning to the left I often feel vertigo and have lost balance; when this happens to be a stair case, the whole thing feels unstable and like it’s rocking back and forth while I step up. I have a constant sense of drainage in my right throat area. If I turn left too fast I get a lightning strike behind right mastoid area.
This is a lot, I know, and I’m hopeful something may resonate. I’m exhausted and it’s too many symptoms to even remember/share for a single appointment – the docs glaze over as much as I do, it’s a lot. And yet it definitely seems very stylohyoid chain adjacent, if not on the money.
I wish I had better words for my existing doctors, or a doctor to visit familiar with these symptoms, if they’re sufficiently connected. Here are some scans for those interested, maybe someone has some ideas I can share with one of my doctors. I’m definitely at a loss and the pain constant and debilitating.
Thanks so much yall.
TLDR: I stress-typed out a novel explaining my ~20 year journey accumulating the following right-sided symptoms:
EAR/HEARING:
-
Lifelong right ear pain
-
Tinnitus (constant, since teens)
-
Pulsatile tinnitus when eating/swallowing/wearing headphones
-
Ear fullness, tickling, and tingling sensations
-
Brief episodes (10-20 seconds) of ear fullness with heavy ringing and temporary deafness
EYES/VISION:
-
Right eye pain
-
Visual distortions (pulsing vision, trouble holding gaze on details)
-
Visual snow syndrome (seeing dots)
-
Flashes of white light in corner of vision
-
World pulses with each heartbeat
-
When bending over: right eye feels punched from behind
-
Feeling like right eye wants to roll back
-
Dry eye
HEAD/FACE:
-
Right facial pain (general)
-
Heavy head feeling
-
Pain in back of head/upper neck
-
Throbbing in right eye/cheek/upper clavicle/ear area
-
When bending over: right face throbs
-
Regular pulsations in right face/head/neck
-
Pain radiating up cheeks/cheekbones/temples
JAW:
-
Charlie horses under right jaw
-
Right jaw feels like it’s hanging at the joint
-
Resting tongue between teeth to stabilize jaw
NECK/THROAT/SWALLOWING:
-
Difficulty swallowing properly on right side
-
Food feels stuck
-
Choking sensation when turning head right (very strong)
-
Stabbing/pulling/object sensations in right neck
-
Pain radiating to lower tongue, gums
-
Light pressure on right neck feels like choking
-
Constant drainage sensation in right throat area
-
Pain on swallowing (nearly always)
-
Lightning strike sensation behind right mastoid when turning left quickly
CHEST/BREATHING:
- Right lung won’t inflate fully at base
MUSCULOSKELETAL:
-
Pain stretching down to shoulder
-
Constant pulsations in clavicle/shoulder area (especially when lying on right side)
-
Significant atrophy in upper right shoulder/back
-
Can’t sleep through night due to neck discomfort
NEUROLOGICAL/BALANCE:
-
Vertigo (being pulled backwards)
-
Vertigo and loss of balance when body turning left
-
Stairs feel unstable/rocking when body turning left
POSITIONAL/TRIGGERS:
-
All symptoms worse when lying down
-
Symptoms worse when lying on right side
-
Symptoms triggered by bending over
-
Symptoms triggered by turning head right